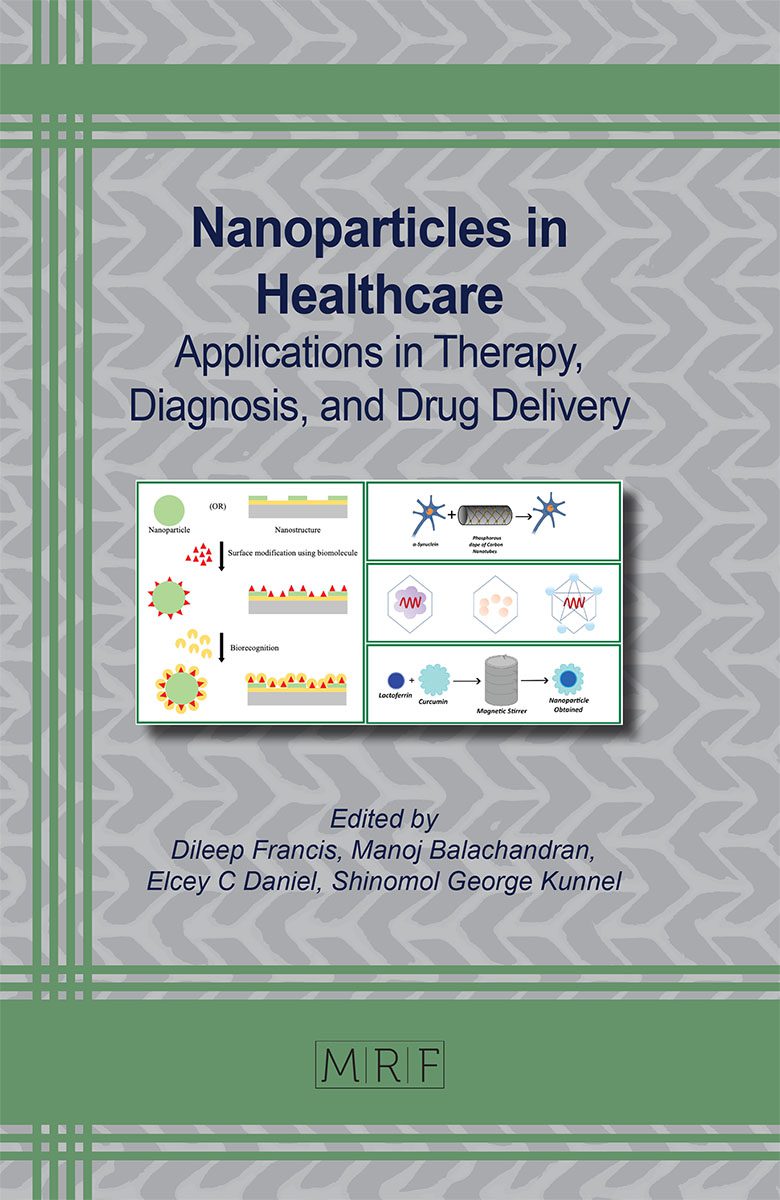
Overview of Nanotechnology Applications in Healthcare
Tejaswini Ronur Praful
Microorganisms gaining drug resistance, difficulty in disease screening, unavailability of point-of-care diagnostic tools are few challenges in the healthcare industry. Over the past few decades, much research has been directed towards developing new nanomaterials with tunable properties for diverse applications in biomedicine, bioimaging, disease diagnosis, therapeutic formulations, etc. Nanosystems specifically used in the healthcare sector include specially designed and functionalized nanomaterials for suitable applications. Nanotechnology finds important applications in identification of specific types of cancers even before their onset, identification of specific infections, targeted gene and drug delivery systems, etc.
Keywords
Nanoparticle, Nanostructure, Nanomaterial, Nanosystems, Functionalization, Healthcare, Diagnosis, Imaging, Biomedicine, Therapy
Published online 2/10/2024, 23 pages
Citation: Tejaswini Ronur Praful, Overview of Nanotechnology Applications in Healthcare, Materials Research Foundations, Vol. 160, pp 1-23, 2024
DOI: https://doi.org/10.21741/9781644902974-1
Part of the book on Nanoparticles in Healthcare
References
[1] Information on https://www.weforum.org/agenda/2023/04/world-health-day-healthcare-trends/
[2] Information on https://www.who.int/docs/default-source/documents/gs4dhdaa2a9f352b0445bafbc79ca799dce4d.pdf
[3] Syedmoradi, L., Daneshpour, M., Alvandipour, M., Gomez, F. A., Hajghassem, H., & Omidfar, K. (2017). Point of care testing: The impact of nanotechnology. Biosensors & bioelectronics, 87, 373-387. https://doi.org/10.1016/j.bios.2016.08.084 https://doi.org/10.1016/j.bios.2016.08.084
[4] Nouailhat, A. (2010). An introduction to nanoscience and nanotechnology (Vol. 10). John Wiley & Sons.
[5] Joachim, C. (2005). To be nano or not to be nano?. Nature Materials, 4(2), 107-109. https://doi.org/10.1038/nmat1319
[6] Bhattacharyya, S., Sandhu, K., & Chockalingam, S. (2023). Nanotechnology-based healthcare engineering products and recent patents-an update. In Emerging Nanotechnologies for Medical Applications (pp. 273-296). Elsevier. https://doi.org/10.1016/B978-0-323-91182-5.00004-8
[7] Sahoo, S. K., Parveen, S., & Panda, J. J. (2007). The present and future of nanotechnology in human health care. Nanomedicine: Nanotechnology, biology and medicine, 3(1), 20-31. https://doi.org/10.1016/j.nano.2006.11.008
[8] Shahcheraghi, N., Golchin, H., Sadri, Z., Tabari, Y., Borhanifar, F., & Makani, S. (2022). Nano-biotechnology, an applicable approach for sustainable future. 3 Biotech, 12(3), 65. https://doi.org/10.1007/s13205-021-03108-9
[9] Verma, S. K., Suar, M., & Mishra, Y. K. (2022). Green Perspective of Nano-Biotechnology: Nanotoxicity Horizon to Biomedical Applications. Frontiers in Bioengineering and Biotechnology, 10. https://doi.org/10.3389/fbioe.2022.919226
[10] Yan, Y., Zhu, X., Yu, Y., Li, C., Zhang, Z., & Wang, F. (2022). Nanotechnology strategies for plant genetic engineering. Advanced Materials, 34(7), 2106945. https://doi.org/10.1002/adma.202106945
[11] Squire, H. J., Tomatz, S., Voke, E., González-Grandío, E., & Landry, M. (2023). The emerging role of nanotechnology in plant genetic engineering. Nature Reviews Bioengineering, 1-15. https://doi.org/10.1038/s44222-023-00037-5
[12] Huang, X., Kon, E., Han, X., Zhang, X., Kong, N., Mitchell, M. J., Dan, P., & Tao, W. (2022). Nanotechnology-based strategies against SARS-CoV-2 variants. Nature Nanotechnology, 17(10), 1027-1037. https://doi.org/10.1038/s41565-022-01174-5
[13] Gildiz, S., & Minko, T. (2023). Nanotechnology-based nucleic acid vaccines for treatment of ovarian cancer. Pharmaceutical research, 40(1), 123-144. https://doi.org/10.1007/s11095-022-03434-4
[14] Kiremitler, N. B., Kemerli, M. Z., Kayaci, N., Karagoz, S., Pekdemir, S., Sarp, G., … & Yilmaz, E. (2022). Nanostructures for the prevention, diagnosis, and treatment of SARS-CoV-2: A review. ACS Applied Nano Materials, 5(5), 6029-6054. https://doi.org/10.1021/acsanm.2c00181
[15] Ayub, A., & Wettig, S. (2022). An overview of nanotechnologies for drug delivery to the brain. Pharmaceutics, 14(2), 224. https://doi.org/10.3390/pharmaceutics14020224
[16] Hamimed, S., Jabberi, M., & Chatti, A. (2022). Nanotechnology in drug and gene delivery. Naunyn-schmiedeberg’s Archives of Pharmacology, 395(7), 769-787. https://doi.org/10.1007/s00210-022-02245-z
[17] Manikandan, S., Subbaiya, R., Saravanan, M., Ponraj, M., Selvam, M., & Pugazhendhi, A. (2022). A critical review of advanced nanotechnology and hybrid membrane based water recycling, reuse, and wastewater treatment processes. Chemosphere, 289, 132867. https://doi.org/10.1016/j.chemosphere.2021.132867
[18] Jain, S., Gupta, I., Walia, P., & Swami, S. (2022). Application of Actinobacteria in Agriculture, Nanotechnology, and Bioremediation. In Actinobacteria-Diversity, Applications and Medical Aspects. IntechOpen. https://doi.org/10.5772/intechopen.104385
[19] Gowda, G. N., Zhang, S., Gu, H., Asiago, V., Shanaiah, N., & Raftery, D. (2008). Metabolomics-based methods for early disease diagnostics. Expert review of molecular diagnostics, 8(5), 617-633. https://doi.org/10.1586/14737159.8.5.617
[20] Kim, B. Y., Rutka, J. T., & Chan, W. C. (2010). Nanomedicine. New England Journal of Medicine, 363(25), 2434-2443. https://doi.org/10.1056/NEJMra0912273
[21] Riehemann, K., Schneider, S. W., Luger, T. A., Godin, B., Ferrari, M., & Fuchs, H. (2009). Nanomedicine-challenge and perspectives. Angewandte Chemie International Edition, 48(5), 872-897. https://doi.org/10.1002/anie.200802585
[22] Chen, H., Zhang, W., Zhu, G., Xie, J., & Chen, X. (2017). Rethinking cancer nanotheranostics. Nature Reviews Materials, 2(7), 1-18. https://doi.org/10.1038/natrevmats.2017.24
[23] Sharma, A. K. (2023). Current Trends in Nanotheranostics: A Concise Review on Bioimaging and Smart Wearable Technology. Nanotheranostics, 7(3), 258-269. https://doi.org/10.7150/ntno.82886
[24] Pirzada, M., & Altintas, Z. (2019). Nanomaterials for healthcare biosensing applications. Sensors, 19(23), 5311. https://doi.org/10.3390/s19235311
[25] Xie, L., Zhang, Z., Wu, Q., Gao, Z., Mi, G., Wang, R., … & Du, Y. (2023). Intelligent wearable devices based on nanomaterials and nanostructures for healthcare. Nanoscale. https://doi.org/10.1039/D2NR04551F
[26] Schwab, F., Rothen-Rutishauser, B., & Petri-Fink, A. (2020). When plants and plastic interact. Nature Nanotechnology, 15(9), 729-730. https://doi.org/10.1038/s41565-020-0762-x
[27] Yılmaz, D., Günaydın, B. N., & Yüce, M. (2022). Nanotechnology in food and water security: On-site detection of agricultural pollutants through surface-enhanced Raman spectroscopy. Emergent Materials, 5(1), 105-132. https://doi.org/10.1007/s42247-022-00376-w
[28] Iqbal, P., Preece, J. A., & Mendes, P. M. (2012). Nanotechnology: the “top‐down” and “bottom‐up” approaches. Supramolecular chemistry: from molecules to nanomaterials. https://doi.org/10.1002/9780470661345.smc195
[29] Srivastava, S., Bhargava, A., Srivastava, S., & Bhargava, A. (2022). Green nanotechnology: an overview. Green Nanoparticles: The Future of Nanobiotechnology, 1-13. https://doi.org/10.1007/978-981-16-7106-7_1
[30] Anjum, S., Ishaque, S., Fatima, H., Farooq, W., Hano, C., Abbasi, B. H., & Anjum, I. (2021). Emerging applications of nanotechnology in healthcare systems: Grand challenges and perspectives. Pharmaceuticals, 14(8), 707. https://doi.org/10.3390/ph14080707
[31] Oliveira Jr, O. N., Caseli, L., & Ariga, K. (2022). The past and the future of Langmuir and Langmuir-Blodgett films. Chemical Reviews, 122(6), 6459-6513. https://doi.org/10.1021/acs.chemrev.1c00754
[32] Capel, A. J., Rimington, R. P., Lewis, M. P., & Christie, S. D. (2018). 3D printing for chemical, pharmaceutical and biological applications. Nature Reviews Chemistry, 2(12), 422-436. https://doi.org/10.1038/s41570-018-0058-y
[33] Charbgoo, F., Ahmad, M. B., & Darroudi, M. (2017). Cerium oxide nanoparticles: green synthesis and biological applications. International journal of nanomedicine, 12, 1401. https://doi.org/10.2147/IJN.S124855
[34] Pansambal, S., Oza, R., Borgave, S., Chauhan, A., Bardapurkar, P., Vyas, S., & Ghotekar, S. (2022). Bioengineered cerium oxide (CeO2) nanoparticles and their diverse applications: a review. Applied Nanoscience, 1-26. https://doi.org/10.1007/s13204-022-02574-8
[35] Lo, W. S., Kwok, W. M., Law, G. L., Yeung, C. T., Chan, C. T. L., Yeung, H. L., Kong, H. K., Chen, C. H., Murphy, M. B., Wong, K. L., & Wong, W. T. (2011). Impressive europium red emission induced by two-photon excitation for biological applications. Inorganic chemistry, 50(12), 5309-5311. https://doi.org/10.1021/ic102465j
[36] Londhe, S., & Patra, C. R. (2022). Biomedical applications of europium hydroxide nanorods. Nanomedicine, 17(1), 5-8. https://doi.org/10.2217/nnm-2021-0351
[37] Ishikawa, I., Aoki, A., & Takasaki, A. A. (2004). Potential applications of Erbium: YAG laser in periodontics. Journal of periodontal research, 39(4), 275-285. https://doi.org/10.1111/j.1600-0765.2004.00738.x
[38] Mondal, S., Park, S., Choi, J., Tran, L. H., Yi, M., Shin, J. H., … & Oh, J. (2020). Bioactive, luminescent erbium-doped hydroxyapatite nanocrystals for biomedical applications. Ceramics international, 46(10), 16020-16031. https://doi.org/10.1016/j.ceramint.2020.03.152
[39] Rajeshkumar, S., & Naik, P. (2018). Synthesis and biomedical applications of cerium oxide nanoparticles-a review. Biotechnology Reports, 17, 1-5. https://doi.org/10.1016/j.btre.2017.11.008
[40] Barker, E., Shepherd, J., & Asencio, I. O. (2022). The use of cerium compounds as antimicrobials for biomedical applications. Molecules, 27(9), 2678. https://doi.org/10.3390/molecules27092678
[41] De, M., Ghosh, P. S., & Rotello, V. M. (2008). Applications of nanoparticles in biology. Advanced Materials, 20(22), 4225-4241. https://doi.org/10.1002/adma.200703183
[42] Schultz, D. A. (2003). Plasmon resonant particles for biological detection. Current opinion in biotechnology, 14(1), 13-22. https://doi.org/10.1016/S0958-1669(02)00015-0
[43] Nakamura, S., Sato, M., Sato, Y., Ando, N., Takayama, T., Fujita, M., & Ishihara, M. (2019). Synthesis and application of silver nanoparticles (Ag NPs) for the prevention of infection in healthcare workers. International journal of molecular sciences, 20(15), 3620. https://doi.org/10.3390/ijms20153620
[44] Dhayalan, M., Karikalan, P., Riyaz Savaas Umar, M., & Srinivasan, N. (2021). Biomedical Applications of Silver Nanoparticles. IntechOpen. doi: 10.5772/intechopen.99367 https://doi.org/10.5772/intechopen.99367
[45] Guo, C., Sun, L., Chen, X., & Zhang, D. (2013). Oxidative stress, mitochondrial damage and neurodegenerative diseases. Neural regeneration research, 8(21), 2003.
[46] Wang, L., Hu, C., & Shao, L. (2017). The antimicrobial activity of nanoparticles: present situation and prospects for the future. International journal of nanomedicine, 12, 1227. https://doi.org/10.2147/IJN.S121956
[47] Botteon, C. E. A., Silva, L. B., Ccana-Ccapatinta, G. V., Silva, T. S., Ambrosio, S. R., Veneziani, R. C. S., Bastos, J. K., & Marcato, P. D. (2021). Biosynthesis and characterization of gold nanoparticles using Brazilian red propolis and evaluation of its antimicrobial and anticancer activities. Scientific Reports, 11(1), 1974. https://doi.org/10.1038/s41598-021-81281-w
[48] Ratan, Z. A., Haidere, M. F., Nurunnabi, M. D., Shahriar, S. M., Ahammad, A. S., Shim, Y. Y., Martin, J. T. R., & Cho, J. Y. (2020). Green chemistry synthesis of silver nanoparticles and their potential anticancer effects. Cancers, 12(4), 855. https://doi.org/10.3390/cancers12040855
[49] Xu, L., Yi-Yi, W., Huang, J., Chun-Yuan, C., Zhen-Xing, W., & Xie, H. (2020). Silver nanoparticles: Synthesis, medical applications and biosafety. Theranostics, 10(20), 8996. https://doi.org/10.7150/thno.45413
[50] Hu, X., Zhang, Y., Ding, T., Liu, J., & Zhao, H. (2020). Multifunctional gold nanoparticles: a novel nanomaterial for various medical applications and biological activities. Frontiers in Bioengineering and Biotechnology, 8, 990. https://doi.org/10.3389/fbioe.2020.00990
[51] Large, D. E., Abdelmessih, R. G., Fink, E. A., & Auguste, D. T. (2021). Liposome composition in drug delivery design, synthesis, characterization, and clinical application. Advanced Drug Delivery Reviews, 176, 113851. https://doi.org/10.1016/j.addr.2021.113851
[52] Hainfeld, J. F., Furuya, F. R., & Powell, R. D. (1999). Metallosomes. Journal of Structural Biology, 127(2), 152-160. doi:10.1006/jsbi.1999.4145 https://doi.org/10.1006/jsbi.1999.4145
[53] Bokov, D., Turki Jalil, A., Chupradit, S., Suksatan, W., Javed Ansari, M., Shewael, I. H., Valiev, G. H., & Kianfar, E. (2021). Nanomaterial by sol-gel method: synthesis and application. Advances in Materials Science and Engineering, 2021, 1-21. https://doi.org/10.1155/2021/5102014
[54] Yilmaz, E., & Soylak, M. (2020). Functionalized nanomaterials for sample preparation methods. In Handbook of Nanomaterials in analytical chemistry (pp. 375-413). Elsevier. https://doi.org/10.1016/B978-0-12-816699-4.00015-3
[55] Aguilar, G. V. (2018). Introductory chapter: a brief semblance of the sol-gel method in research. Sol-Gel Method-Design and Synthesis of New Materials with Interesting Physical, Chemical and Biological Properties.
[56] Thompson, L. F. (1983). An introduction to lithography. https://doi.org/10.1021/bk-1983-0219.ch001
[57] Xia, Y., & Whitesides, G. M. (1998). Soft lithography. Annual review of materials science, 28(1), 153-184. https://doi.org/10.1146/annurev.matsci.28.1.153
[58] Zhang, S. (2003). Fabrication of novel biomaterials through molecular self-assembly. Nature biotechnology, 21(10), 1171-1178. https://doi.org/10.1038/nbt874
[59] Whitesides, G. M., Mathias, J. P., & Seto, C. T. (1991). Molecular self-assembly and nanochemistry: a chemical strategy for the synthesis of nanostructures. Science, 254(5036), 1312-1319. https://doi.org/10.1126/science.1962191
[60] Kajtez, J., Buchmann, S., Vasudevan, S., Birtele, M., Rocchetti, S., Pless, C. J., Heiskanen, A., Barker, R.A., Martínez‐Serrano, A., Parmar, M. & Emnéus, J. (2020). 3D‐printed soft lithography for complex compartmentalized microfluidic neural devices. Advanced Science, 7(16), 2001150. https://doi.org/10.1002/advs.202001150
[61] Roweis, S., Winfree, E., Burgoyne, R., Chelyapov, N. V., Goodman, M. F., Rothemund, P. W., & Adleman, L. M. (1998). A sticker-based model for DNA computation. Journal of Computational Biology, 5(4), 615-629. https://doi.org/10.1089/cmb.1998.5.615
[62] Dey, S., Fan, C., Gothelf, K. V., Li, J., Lin, C., Liu, L., … & Zhan, P. (2021). DNA origami. Nature Reviews Methods Primers, 1(1), 13. https://doi.org/10.1038/s43586-020-00009-8
[63] Kasthuri, A. (2018). Challenges to healthcare in India-The five A’s. Indian journal of community medicine: official publication of Indian Association of Preventive & Social Medicine, 43(3), 141.
[64] Sperling, R. A., & Parak, W. J. (2010). Surface modification, functionalization and bioconjugation of colloidal inorganic nanoparticles. Philosophical Transactions of the Royal Society A: Mathematical, Physical and Engineering Sciences, 368(1915), 1333-1383. https://doi.org/10.1098/rsta.2009.0273
[65] Vavrinsky, E., Esfahani, N. E., Hausner, M., Kuzma, A., Rezo, V., Donoval, M., & Kosnacova, H. (2022). The current state of optical sensors in medical wearables. Biosensors, 12(4), 217. https://doi.org/10.3390/bios12040217
[66] Chen, S., Qi, J., Fan, S., Qiao, Z., Yeo, J. C., & Lim, C. T. (2021). Flexible wearable sensors for cardiovascular health monitoring. Advanced Healthcare Materials, 10(17), 2100116. https://doi.org/10.1002/adhm.202100116
[67] Wu, J., Dong, M., Rigatto, C., Liu, Y., & Lin, F. (2018). Lab-on-chip technology for chronic disease diagnosis. NPJ digital medicine, 1(1), 7. https://doi.org/10.1038/s41746-017-0014-0
[68] Hou, T., Chang, H., Jiang, H., Wang, P., Li, N., Song, Y., & Li, D. (2022). Smartphone based microfluidic lab-on-chip device for real-time detection, counting and sizing of living algae. Measurement, 187, 110304. https://doi.org/10.1016/j.measurement.2021.110304
[69] Miller, M. B., & Tang, Y. W. (2009). Basic concepts of microarrays and potential applications in clinical microbiology. Clinical microbiology reviews, 22(4), 611-633. https://doi.org/10.1128/CMR.00019-09 https://doi.org/10.1128/CMR.00019-09
[70] Dang, X., Bardhan, N. M., Qi, J., Gu, L., Eze, N. A., Lin, C. W., Kataria, S. Hammond, P. T., & Belcher, A. M. (2019). Deep-tissue optical imaging of near cellular-sized features. Scientific reports, 9(1), 1-12. https://doi.org/10.1038/s41598-019-39502-w
[71] Appel, A. A., Anastasio, M. A., Larson, J. C., & Brey, E. M. (2013). Imaging challenges in biomaterials and tissue engineering. Biomaterials, 34(28), 6615-6630. https://doi.org/10.1016/j.biomaterials.2013.05.033
[72] Ho, S. L., Yue, H., Tegafaw, T., Ahmad, M. Y., Liu, S., Nam, S. W., Chang, Y., & Lee, G. H. (2022). Gadolinium neutron capture therapy (GdNCT) agents from molecular to nano: Current status and perspectives. ACS omega, 7(3), 2533-2553. https://doi.org/10.1021/acsomega.1c06603
[73] Marasini, R., Thanh Nguyen, T. D., & Aryal, S. (2020). Integration of gadolinium in nanostructure for contrast enhanced-magnetic resonance imaging. Wiley interdisciplinary reviews. Nanomedicine and nanobiotechnology, 12(1), e1580. https://doi.org/10.1002/wnan.1580
[74] Cai, X., Zhu, Q., Zeng, Y., Zeng, Q., Chen, X., & Zhan, Y. (2019). Manganese Oxide Nanoparticles As MRI Contrast Agents In Tumor Multimodal Imaging And Therapy. International journal of nanomedicine, 14, 8321-8344. https://doi.org/10.2147/IJN.S218085
[75] Kunuku, S., Lin, B. R., Chen, C. H., Chang, C. H., Chen, T. Y., Hsiao, T. Y., Yu, H.K., Chang, Y.J., Liao, L.C., Chen, F.H., & Niu, H. (2023). Nanodiamonds Doped with Manganese for Applications in Magnetic Resonance Imaging. ACS omega, 8(4), 4398-4409. https://doi.org/10.1021/acsomega.2c08043
[76] Chen, C., Ge, J., Gao, Y., Chen, L., Cui, J., Zeng, J., & Gao, M. (2022). Ultrasmall superparamagnetic iron oxide nanoparticles: A next generation contrast agent for magnetic resonance imaging. Wiley Interdisciplinary Reviews: Nanomedicine and Nanobiotechnology, 14(1), e1740. https://doi.org/10.1002/wnan.1740
[77] Geppert, M., & Himly, M. (2021). Iron oxide nanoparticles in bioimaging – an immune perspective. Frontiers in Immunology, 12. https://doi.org/10.3389/fimmu.2021.688927
[78] Chen, X., & Wong, S. (Eds.). (2014). Cancer theranostics. Academic Press. https://doi.org/10.1016/B978-0-12-407722-5.00001-3
[79] Iravani, S., & Varma, R. S. (2022). MXenes in cancer nanotheranostics. Nanomaterials, 12(19), 3360. https://doi.org/10.3390/nano12193360
[80] Ladju, R. B., Ulhaq, Z. S., & Soraya, G. V. (2022). Nanotheranostics: A powerful next-generation solution to tackle hepatocellular carcinoma. World journal of gastroenterology, 28(2), 176-187. https://doi.org/10.3748/wjg.v28.i2.176
[81] Chavda, V. P., Balar, P. C., & Patel, S. B. (2023). Interventional nanotheranostics in hepatocellular carcinoma. Nanotheranostics, 7(2), 128-141. https://doi.org/10.7150/ntno.80120
[82] Cao, L., Zhu, Y. Q., Wu, Z. X., Wang, G. X., & Cheng, H. W. (2021). Engineering nanotheranostic strategies for liver cancer. World journal of gastrointestinal oncology, 13(10), 1213-1228. https://doi.org/10.4251/wjgo.v13.i10.1213
[83] Koudelka, K. J., Pitek, A. S., Manchester, M., & Steinmetz, N. F. (2015). Virus-Based Nanoparticles as Versatile Nanomachines. Annual review of virology, 2(1), 379-401. https://doi.org/10.1146/annurev-virology-100114-055141
[84] Guenther, C. M., Kuypers, B. E., Lam, M. T., Robinson, T. M., Zhao, J., & Suh, J. (2014). Synthetic virology: engineering viruses for gene delivery. Wiley Interdisciplinary Reviews: Nanomedicine and Nanobiotechnology, 6(6), 548-558. https://doi.org/10.1002/wnan.1287
[85] Tariq, H., Batool, S., Asif, S., Ali, M., & Abbasi, B. H. (2022). Virus-like particles: Revolutionary platforms for developing vaccines against emerging infectious diseases. Frontiers in microbiology, 12, 4137. https://doi.org/10.3389/fmicb.2021.790121
[86] Nooraei, S., Bahrulolum, H., Hoseini, Z. S., Katalani, C., Hajizade, A., Easton, A. J., & Ahmadian, G. (2021). Virus-like particles: Preparation, immunogenicity and their roles as nanovaccines and Drug Nanocarriers. Journal of Nanobiotechnology, 19(1). https://doi.org/10.1186/s12951-021-00806-7
[87] Peabody, D. S., Peabody, J., Bradfute, S. B., & Chackerian, B. (2021). RNA Phage VLP-Based Vaccine Platforms. Pharmaceuticals (Basel, Switzerland), 14(8), 764. https://doi.org/10.3390/ph14080764
[88] Soto, F., Wang, J., Ahmed, R., & Demirci, U. (2020). Medical micro/nanorobots in precision medicine. Advanced Science, 7(21), 2002203. https://doi.org/10.1002/advs.202002203
[89] Hortelão, A. C., Patiño, T., Perez‐Jiménez, A., Blanco, À., & Sánchez, S. (2018). Enzyme‐powered nanobots enhance anticancer drug delivery. Advanced Functional Materials, 28(25), 1705086. https://doi.org/10.1002/adfm.201705086
[90] Feng, Y., An, M., Liu, Y., Sarwar, M. T., & Yang, H. (2023). Advances in Chemically Powered Micro/Nanorobots for Biological Applications: A Review. Advanced Functional Materials, 33(1), 2209883. https://doi.org/10.1002/adfm.202209883
[91] Information on https://builtin.com/robotics/nanorobotics
[92] Kim, J., Campbell, A. S., de Ávila, B. E.-F., & Wang, J. (2019). Wearable biosensors for healthcare monitoring. Nature Biotechnology, 37(4), 389-406. https://doi.org/10.1038/s41587-019-0045-y
[93] Information on https://lifesignals.com/wearable-biosensors/
[94] Sharma, A., Badea, M., Tiwari, S., & Marty, J. L. (2021). Wearable Biosensors: An Alternative and Practical Approach in Healthcare and Disease Monitoring. Molecules (Basel, Switzerland), 26(3), 748. https://doi.org/10.3390/molecules26030748
[95] Bhalla, N., Jolly, P., Formisano, N., & Estrela, P. (2016). Introduction to biosensors. Essays in biochemistry, 60(1), 1-8. https://doi.org/10.1042/EBC20150001