Application of Biodegradable Lipid Composites in Drug Delivery
Vishal Beldar, Ritika Joshi, Sujit Kumar Ghosh and Manojkumar Jadhao
With the advent of nanotechnology, considerable advancements in the realm of drug delivery have been witnessed with respect to improvements in drug efficacy and safety. Among the various novel drug delivery systems, lipid-based excipients have demonstrated clinical benefit till date. However, parameters like aqueous solubility, permeability, stability, and targeting, in addition to the design of sustainable lipid based drug delivery platforms, still pose a challenge for the researchers. The most recent developments, using lipid composites, have been focused on these issues. Hence this chapter highlights the myriad of lipid composites implemented as drug delivery carriers against lethal diseases and unfolds the promising future of these platforms in nanomedicine research.
Keywords
Drug Delivery, Lipids, Liposomes, Nanomaterials, Lipid Composites
Published online 2/15/2020, 40 pages
Citation: Vishal Beldar, Ritika Joshi, Sujit Kumar Ghosh and Manojkumar Jadhao, Application of Biodegradable Lipid Composites in Drug Delivery, Materials Research Foundations, Vol. 68, pp 156-195, 2020
DOI: https://doi.org/10.21741/9781644900659-7
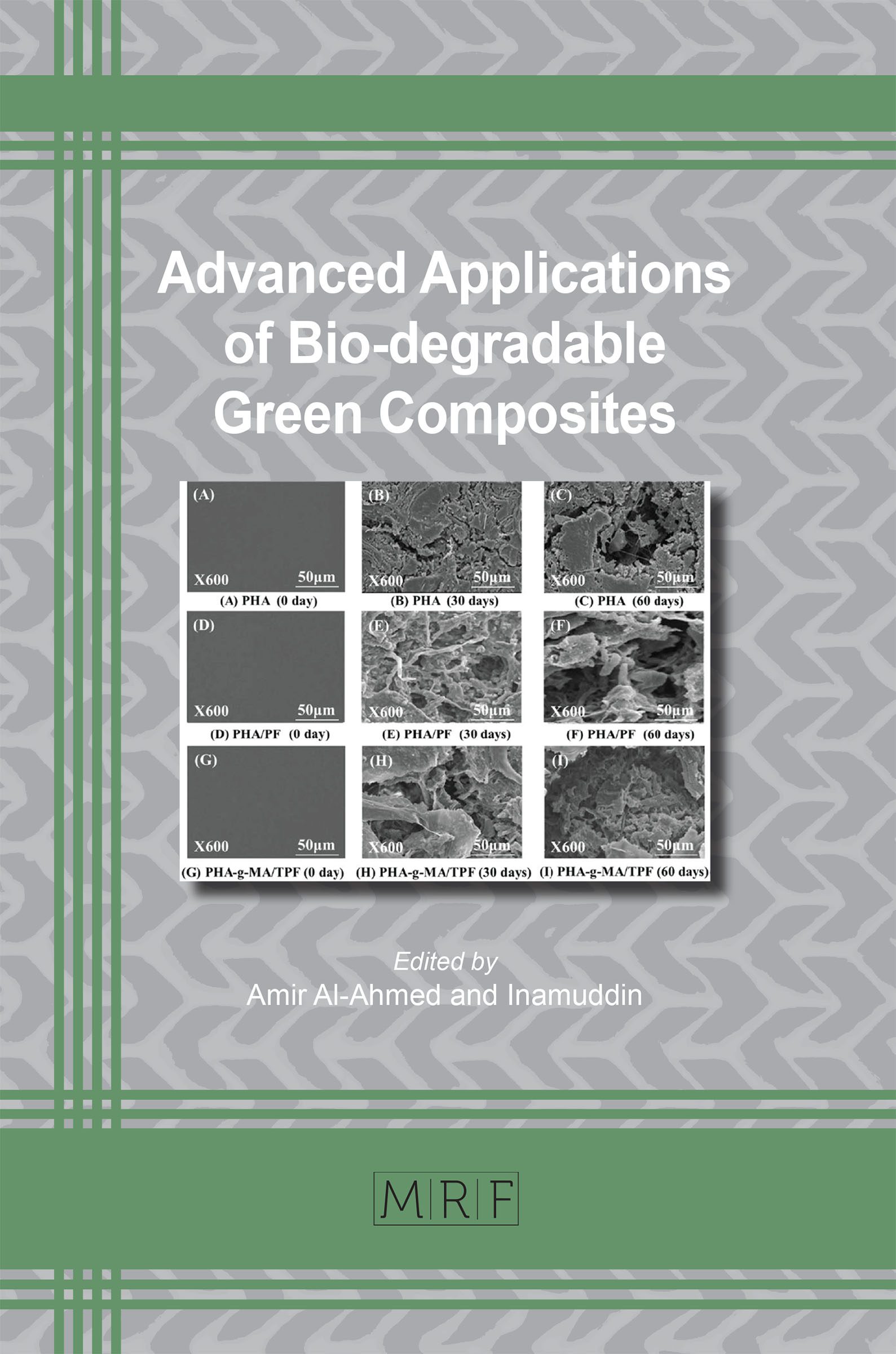
Part of the book on Advanced Applications of Bio-degradable Green Composites
References
[1] K.K. Jain, Current Status and Future Prospects of Drug Delivery Systems, in: Drug Deliv. Syst., Academic, Humana Press, New York, NY, 2014: pp. 1–56. https://doi.org/10.1007/978-1-4939-0363-4_1
[2] P. Pàmies, A. Stoddart, Materials for drug delivery, Nat. Mater. 12 (2013) 957–957. https://doi.org/10.1038/nmat3798
[3] B.J. Boyd, T.H. Nguyen, A. Müllertz, Lipids in Oral Controlled Release Drug Delivery, in: Control. Release Oral Drug Deliv., Springer US, Boston, MA, 2011: pp. 299–327. https://doi.org/10.1007/978-1-4614-1004-1_15
[4] A.T. Florence, A Short History of Controlled Drug Release and an Introduction, in: Control. Release Oral Drug Deliv., Springer US, Boston, MA, 2011: pp. 1–26. https://doi.org/10.1007/978-1-4614-1004-1_1
[5] J. Reinholz, K. Landfester, V. Mailänder, The challenges of oral drug delivery via nanocarriers, Drug Deliv. 25 (2018) 1694. https://doi.org/10.1080/10717544.2018.1501119
[6] H.D. Williams, N.L. Trevaskis, S.A. Charman, R.M. Shanker, W.N. Charman, C.W. Pouton, C.J.H. Porter, Strategies to address low drug solubility in discovery and development, Pharmacol. Rev. 65 (2013) 315–499. https://doi.org/10.1124/PR.112.005660
[7] R.L. Carrier, L.A. Miller, I. Ahmed, The utility of cyclodextrins for enhancing oral bioavailability, J. Control. Release. 123 (2007) 78–99. https://doi.org/10.1016/J.JCONREL.2007.07.018
[8] S. Kalepu, V. Nekkanti, Insoluble drug delivery strategies: Review of recent advances and business prospects, Acta Pharm. Sin. B. 5 (2015) 442–453. https://doi.org/10.1016/J.APSB.2015.07.003
[9] S. Banerjee, A. Kundu, Lipid-drug conjugates: a potential nanocarrier system for oral drug delivery applications, DARU J. Pharm. Sci. 26 (2018) 65–75. https://doi.org/10.1007/s40199-018-0209-1
[10] D. Irby, C. Du, F. Li, Lipid–drug conjugate for enhancing drug delivery, Mol. Pharm. 14 (2017) 1325–1338. https://doi.org/10.1021/acs.molpharmaceut.6b01027
[11] R.H. Müller, M. Radtke, S.A. Wissing, Solid lipid nanoparticles (SLN) and nanostructured lipid carriers (NLC) in cosmetic and dermatological preparations, Adv. Drug Deliv. Rev. 54 (2002) S131–S155. https://doi.org/10.1016/S0169-409X(02)00118-7
[12] M. Jadhao, P. Ahirkar, H. Kumar, R. Joshi, O.R. Meitei, S.K. Ghosh, Surfactant induced aggregation-disaggregation of photodynamic active chlorin e6 and its relevant interaction with DNA alkylating quinone in a biomimic micellar microenvironment, RSC Adv. 5 (2015). https://doi.org/10.1039/c5ra16181a
[13] M. Jadhao, R. Joshi, K. Ganorkar, S.K. Ghosh, Biomimetic systems trigger a benzothiazole based molecular switch to ‘turn on’ fluorescence, Spectrochim. Acta Part A Mol. Biomol. Spectrosc. 217 (2019) 197–205. https://doi.org/10.1016/J.SAA.2019.03.089
[14] S. Cikrikci, B. Mert, M.H. Oztop, Development of ph sensitive alginate/gum tragacanth based hydrogels for oral insulin delivery, J. Agric. Food Chem. 66 (2018) 11784–11796. https://doi.org/10.1021/acs.jafc.8b02525
[15] D.G. Wallace, J. Rosenblatt, Collagen gel systems for sustained delivery and tissue engineering, Adv. Drug Deliv. Rev. 55 (2003) 1631–1649. https://doi.org/10.1016/J.ADDR.2003.08.004
[16] B. Chatin, M. Mével, J. Devallière, L. Dallet, T. Haudebourg, P. Peuziat, T. Colombani, M. Berchel, O. Lambert, A. Edelman, B. Pitard, Liposome-based Formulation for intracellular delivery of functional proteins, Mol. Ther. Nucleic Acids. 4 (2015) 244. https://doi.org/10.1038/MTNA.2015.17
[17] J.C. Byeon, S.E. Lee, T.H. Kim, J. Bin Ahn, D.H. Kim, J.S. Choi, J.S. Park, Design of novel proliposome formulation for antioxidant peptide, glutathione with enhanced oral bioavailability and stability, Drug Deliv. 26 (2019) 216–225. https://doi.org/10.1080/10717544.2018.1551441
[18] B. Garnier, S. Tan, C. Gounou, A.R. Brisson, J. Laroche-Traineau, M.J. Jacobin-Valat, G. Clofent-Sanchez, Development of a Platform of antibody-presenting liposomes, Biointerphases. 7 (2012) 11. https://doi.org/10.1007/s13758-011-0011-9
[19] Wikipedia, Lipid polymorphism, (2018). https://en.wikipedia.org/wiki/Lipid_polymorphism
[20] H. Shrestha, R. Bala, S. Arora, Lipid-Based Drug Delivery Systems, J. Pharm. 2014 (2014) 10
[21] S. Ahmed, A. Gull, M. Aqil, M. Danish Ansari, Y. Sultana, Poloxamer-407 thickened lipid colloidal system of agomelatine for brain targeting: Characterization, brain pharmacokinetic study and behavioral study on Wistar rats, Colloids Surfaces B Biointerfaces. 181(2019) 426-436. https://doi.org/10.1016/j.colsurfb.2019.05.016
[22] T.N.Q. Phan, I. Shahzadi, A. Bernkop-Schnürch, Hydrophobic ion-pairs and lipid-based nanocarrier systems: The perfect match for delivery of BCS class 3 drugs, J. Control. Release. 304 (2019) 146–155. https://doi.org/10.1016/j.jconrel.2019.05.011
[23] N.D.T. Le, P.H.L. Tran, B.J. Lee, T.T.D. Tran, Solid lipid particle-based tablets for buccal delivery: The role of solid lipid particles in drug release, J. Drug Deliv. Sci. Technol. 52 (2019) 96–102. https://doi.org/10.1016/j.jddst.2019.04.037
[24] C.J.H. Porter, C.W. Pouton, J.F. Cuine, W.N. Charman, Enhancing intestinal drug solubilisation using lipid-based delivery systems, Adv. Drug Deliv. Rev. 60 (2008) 673–691. https://doi.org/10.1016/j.addr.2007.10.014
[25] M.R.I. Shishir, L. Xie, C. Sun, X. Zheng, W. Chen, Advances in micro and nano-encapsulation of bioactive compounds using biopolymer and lipid-based transporters, Trends Food Sci. Technol. 78 (2018) 34–60. https://doi.org/10.1016/j.tifs.2018.05.018
[26] M.S. Mufamadi, V. Pillay, Y.E. Choonara, L.C. Du Toit, G. Modi, D. Naidoo, V.M.K. Ndesendo, A Review on Composite Liposomal Technologies for Specialized Drug Delivery, J. Drug Deliv. 2011 (2011) 1–19. https://doi.org/10.1155/2011/939851
[27] A. Jain, D. Thakur, G. Ghoshal, O.P. Katare, U.S. Shivhare, Characterization of microcapsulated beta-carotene formed by complex coacervation using casein and gum tragacanth, Int. J. Biol. Macromol. 87 (2016) 101–113. https://doi.org/10.1016/j.ijbiomac.2016.01.117
[28] L. De Souza, D.A. Madalena, A.C. Pinheiro, J.A. Teixeira, A.A. Vicente, Ó.L. Ramos, Micro- and nano bio-based delivery systems for food applications : In vitro behavior, 243 (2017) 23–45. https://doi.org/10.1016/j.cis.2017.02.010
[29] X. Xu, M.A. Khan, D.J. Burgess, Predicting hydrophilic drug encapsulation inside unilamellar liposomes, Int. J. Pharm. 423 (2012) 410–418. https://doi.org/10.1016/j.ijpharm.2011.12.019
[30] S.M. Jafari, D.J. McClements, Nanotechnology Approaches for Increasing Nutrient Bioavailability, 1st ed., Elsevier Inc., 2017. https://doi.org/10.1016/bs.afnr.2016.12.008
[31] G. Liu, W. Huang, O. Babii, X. Gong, Z. Tian, J. Yang, Y. Wang, R.L. Jacobs, V. Donna, A. Lavasanifar, L. Chen, Novel protein–lipid composite nanoparticles with an inner aqueous compartment as delivery systems of hydrophilic nutraceutical compounds, Nanoscale. 10 (2018) 10629–10640. https://doi.org/10.1039/C8NR01009A
[32] R.K. Harwansh, R. Deshmukh, M.A. Rahman, Nanoemulsion: Promising nanocarrier system for delivery of herbal bioactives, J. Drug Deliv. Sci. Technol. 51 (2019) 224–233. https://doi.org/10.1016/j.jddst.2019.03.006
[33] Y.S.R. Elnaggar, S. Omran, H.A. Hazzah, O.Y. Abdallah, Anionic versus cationic bilosomes as oral nanocarriers for enhanced delivery of the hydrophilic drug risedronate, Int. J. Pharm. 564 (2019) 410–425. https://doi.org/10.1016/j.ijpharm.2019.04.069
[34] B.D. Buddy, D. Ratner, Biomaterials science : An introduction to materials in medicine, Academic Press, 2013
[35] A. George, P.A. Shah, P.S. Shrivastav, Natural biodegradable polymers based nano-formulations for drug delivery: A review, Int. J. Pharm. 561 (2019) 244–264. https://doi.org/10.1016/j.ijpharm.2019.03.011
[36] L.N.M. Ribeiro, A.C.S. Alcântara, G.H. Rodrigues da Silva, M. Franz-Montan, S.V.G. Nista, S.R. Castro, V.M. Couto, V.A. Guilherme, E. de Paula, Advances in hybrid polymer-based materials for sustained drug release, Int. J. Polym. Sci. 2017 (2017) 1–16. https://doi.org/10.1155/2017/1231464
[37] Y. Cheng, T. Zou, M. Dai, X.Y. He, N. Peng, K. Wu, X.Q. Wang, C.Y. Liao, Y. Liu, Doxorubicin loaded tumor-triggered targeting ammonium bicarbonate liposomes for tumor-specific drug delivery, Colloids Surfaces B Biointerfaces. 178 (2019) 263–268. https://doi.org/10.1016/j.colsurfb.2019.03.002
[38] Y. Fang, M. Vadlamudi, Y. Huang, X. Guo, Lipid-Coated, pH-Sensitive Magnesium Phosphate Particles for Intracellular Protein Delivery, Pharm. Res. 36 (2019) 81. https://doi.org/10.1007/s11095-019-2607-6
[39] Z. Zhao, W. Yao, N. Wang, C. Liu, H. Zhou, H. Chen, W. Qiao, Synthesis and evaluation of mono- and multi-hydroxyl low toxicity pH-sensitive cationic lipids for drug delivery, Eur. J. Pharm. Sci. 133 (2019) 69–78. https://doi.org/10.1016/j.ejps.2019.03.018
[40] M. Tang, D. Svirskis, E. Leung, M. Kanamala, H. Wang, Z. Wu, Can intracellular drug delivery using hyaluronic acid functionalised pH-sensitive liposomes overcome gemcitabine resistance in pancreatic cancer, J. Control. Release. 305 (2019) 89–100. https://doi.org/10.1016/j.jconrel.2019.05.018
[41] Y. Yao, T. Wang, Y. Liu, N. Zhang, Co-delivery of sorafenib and VEGF-siRNA via pH-sensitive liposomes for the synergistic treatment of hepatocellular carcinoma, Artif. Cells Nanomedicine Biotechnol. 47 (2019) 1374–1383. https://doi.org/10.1080/21691401.2019.1596943
[42] M. Chen, F. Song, Y. Liu, J. Tian, C. Liu, R. Li, Q. Zhang, A dual pH-sensitive liposomal system with charge-reversal and NO generation for overcoming multidrug resistance in cancer, Nanoscale. 11 (2019) 3814–3826. https://doi.org/10.1039/c8nr06218h
[43] G.N. Pawar, N.N. Parayath, A.L. Nocera, B.S. Bleier, M.A. Id, Direct CNS delivery of proteins using thermosensitive liposome-in-gel carrier by heterotopic mucosal engrafting, PLOS ONE. (2018) 1–15
[44] S. Akthar, R.J. Kok, T. Lammers, G. Storm, Influence of cholesterol inclusion on the doxorubicin release characteristics of lysolipid-based thermosensitive liposomes, Int. J. Pharm. (2017). https://doi.org/10.1016/j.ijpharm.2017.11.002
[45] D. Cao, X. Zhang, Y. Luo, H. Wu, X. Ke, F. Group, Liposomal doxorubicin loaded PLGA-PEG-PLGA based thermogel for sustained local drug delivery for the treatment of breast cancer local drug delivery for the treatment of breast cancer, Artif. Cells, Nanomedicine, Biotechnol. 47 (2019) 181–191. https://doi.org/10.1080/21691401.2018.1548470
[46] Y. Mo, H. Du, B. Chen, D. Liu, Q. Yin, Y. Yan, Z. Wang, F. Wan, T. Qi, Y. Wang, Q. Zhang, Y. Wang, Quick-responsive polymer-based thermosensitive liposomes for controlled doxorubicin release and chemotherapy, ACS Biomater. Sci. Eng. 5 (2019) 2316–2329. https://doi.org/10.1021/acsbiomaterials.9b00343
[47] Y.J. Lu, E.Y. Chuang, Y.H. Cheng, T.S. Anilkumar, H.A. Chen, J.P. Chen, Thermosensitive magnetic liposomes for alternating magnetic field-inducible drug delivery in dual targeted brain tumor chemotherapy, Chem. Eng. J. 373 (2019) 720–733. https://doi.org/10.1016/j.cej.2019.05.055
[48] X. Wang, R. Yang, C. Yuan, Y. An, Q. Tang, D. Chen, Preparation of Folic Acid-Targeted Temperature-Sensitive Magnetoliposomes and their Antitumor Effects In Vitro and In Vivo, Targ Oncol. 13 (2018) 481
[49] M. Ayubi, M. Karimi, S. Abdpour, K. Rostamizadeh, M. Parsa, M. Zamani, A. Saedi, Magnetic nanoparticles decorated with PEGylated curcumin as dual targeted drug delivery: Synthesis, toxicity and biocompatibility study, Mater. Sci. Eng. C. 104 (2019) 109810. https://doi.org/10.1016/j.msec.2019.109810
[50] M. Suñé-Pou, M.J. Limeres, I. Nofrerias, A. Nardi-Ricart, S. Prieto-Sánchez, Y. El-Yousfi, P. Pérez-Lozano, E. García-Montoya, M. Miñarro-Carmona, J.R. Ticó, C. Hernández-Munain, C. Suñé, J.M. Suñé-Negre, Improved synthesis and characterization of cholesteryl oleate-loaded cationic solid lipid nanoparticles with high transfection efficiency for gene therapy applications, Colloids Surfaces B Biointerfaces. 180 (2019) 159–167. https://doi.org/10.1016/j.colsurfb.2019.04.037
[51] H.M. Eid, M.H. Elkomy, S.F. El Menshawe, H.F. Salem, Development, optimization, and in vitro/in vivo characterization of enhanced lipid nanoparticles for ocular delivery of ofloxacin: the influence of pegylation and chitosan coating, AAPS PharmSciTech. 20 (2019) 1–14. https://doi.org/10.1208/s12249-019-1371-6
[52] I. Ahmad, J. Pandit, Y. Sultana, A.K. Mishra, P.P. Hazari, M. Aqil, Optimization by design of etoposide loaded solid lipid nanoparticles for ocular delivery: Characterization, pharmacokinetic and deposition study, Mater. Sci. Eng. C. 100 (2019) 959–970. https://doi.org/10.1016/j.msec.2019.03.060
[53] K.Y. Janga, A. Tatke, N. Dudhipala, S.P. Balguri, M.M. Ibrahim, D.N. Maria, M.M. Jablonski, S. Majumdar, Gellan gum based sol-to-gel transforming system of natamycin transfersomes improves topical ocular delivery, J. Pharmacol. Exp. Ther. (2019) jpet.119.256446. https://doi.org/10.1124/jpet.119.256446
[54] G.S. El-feky, M.M. El-naa, A.A. Mahmoud, Journal of Drug Delivery Science and Technology Flexible nano-sized lipid vesicles for the transdermal delivery of colchicine ; in vitro / in vivo investigation, J. Drug Deliv. Sci. Technol. 49 (2019) 24–34. https://doi.org/10.1016/j.jddst.2018.10.036
[55] M.K. Shamshiri, M.K. Shahraky, F. Rahimi, Lecithin soybean phospholipid nano transfersomes as potential carriers for transdermal delivery of the human growth hormone, Journal of Cellular Biochemistry. 120 (2019) 9023-9033. https://doi.org/10.1002/jcb.28176
[56] S. Rajalakshmi, N. Vyawahare, A. Pawar, P. Mahaparale, B. Chellampillai, Current development in novel drug delivery systems of bioactive molecule plumbagin, Artif. Cells, Nanomedicine Biotechnol. 46 (2018) 209–218. https://doi.org/10.1080/21691401.2017.1417865
[57] G.M. El-Zaafarany, M.E. Soliman, S. Mansour, M. Cespi, G.F. Palmieri, L. Illum, L. Casettari, G.A.S. Awad, A tailored thermosensitive PLGA-PEG-PLGA/emulsomes composite for enhanced oxcarbazepine brain delivery via the nasal route, Pharmaceutics. 10 (2018). https://doi.org/10.3390/pharmaceutics10040217
[58] G.M. El-Zaafarany, M.E. Soliman, S. Mansour, G.A.S. Awad, Identifying lipidic emulsomes for improved oxcarbazepine brain targeting: In vitro and rat in vivo studies, Int. J. Pharm. 503 (2016) 127–140. https://doi.org/10.1016/j.ijpharm.2016.02.038
[59] D. Sawant, P.M. Dandagi, A.P. Gadad, Formulation and evaluation of sparfloxacin emulsomes-loaded thermosensitive in situ gel for ophthalmic delivery, J. Sol-Gel Sci. Technol. 77 (2016) 654–665. https://doi.org/10.1007/s10971-015-3897-8
[60] L. Inchaurraga, A.L. Martínez-López, M. Abdulkarim, M. Gumbleton, G. Quincoces, I. Peñuelas, N. Martin-Arbella, J.M. Irache, Modulation of the fate of zein nanoparticles by their coating with a Gantrez® AN-thiamine polymer conjugate, Int. J. Pharm. X. 1 (2019) 100006. https://doi.org/10.1016/j.ijpx.2019.100006
[61] M.J. Costa, J. Kudaravalli, J.T. Ma, W.H. Ho, K. Delaria, C. Holz, A. Stauffer, A.G. Chunyk, Q. Zong, E. Blasi, B. Buetow, T.T. Tran, K. Lindquist, M. Dorywalska, A. Rajpal, D.L. Shelton, P. Strop, S.H. Liu, Optimal design, anti-tumour efficacy and tolerability of anti-CXCR4 antibody drug conjugates, Sci. Rep. 9 (2019) 1–19. https://doi.org/10.1038/s41598-019-38745-x
[62] N. Plenagl, L. Duse, B.S. Seitz, N. Goergen, S.R. Pinnapireddy, J. Jedelska, J. Brüßler, U. Bakowsky, Photodynamic therapy – hypericin tetraether liposome conjugates and their antitumor and antiangiogenic activity, Drug Deliv. 26 (2019) 23–33. https://doi.org/10.1080/10717544.2018.1531954
[63] L.P. Mendes, C. Sarisozen, E. Luther, J. Pan, V.P. Torchilin, Surface-engineered polyethyleneimine-modified liposomes as novel carrier of siRNA and chemotherapeutics for combination treatment of drug-resistant cancers, Drug Deliv. 26 (2019) 443–458. https://doi.org/10.1080/10717544.2019.1574935
[64] K. Kristensen, T.B. Engel, A. Stensballe, J.B. Simonsen, T.L. Andresen, The hard protein corona of stealth liposomes is sparse, J. Control. Release. 307 (2019) 1–15. https://doi.org/10.1016/j.jconrel.2019.05.042
[65] N.S. Awad, V. Paul, M.H. Al-Sayah, G.A. Husseini, Ultrasonically controlled albumin-conjugated liposomes for breast cancer therapy, Artif. Cells, Nanomedicine Biotechnol. 47 (2019) 705–714. https://doi.org/10.1080/21691401.2019.1573175
[66] M.H. Jang, C.H. Kim, H.Y. Yoon, S.W. Sung, M.S. Goh, E.S. Lee, D.J. Shin, Y.W. Choi, Steric stabilization of RIPL peptide-conjugated liposomes and in vitro assessment, J. Pharm. Investig. 49 (2019) 115–125. https://doi.org/10.1007/s40005-018-0392-6
[67] D.D. Lasic, D. Needham, The “Stealth” Liposome: A Prototypical Biomaterial, Chem. Rev. 95 (1995) 2601–2628. https://doi.org/10.1021/cr00040a001
[68] B. Cˇeh, M. Winterhalter, P.M. Frederik, J.J. Vallner, D.D. Lasic, Stealth® liposomes: from theory to product, Adv. Drug Deliv. Rev. 24 (1997) 165–177. https://doi.org/10.1016/S0169-409X(96)00456-5
[69] J. Liu, C. Detrembleur, S. Mornet, C. Jérôme, E. Duguet, Design of hybrid nanovehicles for remotely triggered drug release: An overview, J. Mater. Chem. B. 3 (2015) 6117–6147. https://doi.org/10.1039/C5TB00664C
[70] M. Karimi, A. Ghasemi, P. Sahandi Zangabad, R. Rahighi, S.M. Moosavi Basri, H. Mirshekari, M. Amiri, Z. Shafaei Pishabad, A. Aslani, M. Bozorgomid, D. Ghosh, A. Beyzavi, A. Vaseghi, A.R. Aref, L. Haghani, S. Bahrami, M.R. Hamblin, Smart micro/nanoparticles in stimulus-responsive drug/gene delivery systems, Chem. Soc. Rev. 45 (2016) 1457–1501. https://doi.org/10.1039/C5CS00798D
[71] Y. Matsuzaki, Y. Hamasaki, S.I. Said, pH-Sensitive Liposomes : Possible Clinical Implications, Science. 210 (1980) 1253–1255
[72] S.R. Paliwal, R. Paliwal, S.P. Vyas, A review of mechanistic insight and application of pH-sensitive liposomes in drug delivery, 7544 (2014) 1–12. https://doi.org/10.3109/10717544.2014.882469
[73] S. Mallick, J.S. Choi, Liposomes: Versatile and Biocompatible Nanovesicles for Efficient Biomolecules Delivery, J. Nanosci. Nanotechnol. 14 (2014) 755–765. https://doi.org/10.1166/jnn.2014.9080
[74] S. Mura, J. Nicolas, P. Couvreur, Stimuli-responsive nanocarriers for drug delivery, Nat. Publ. Gr. 12 (2013) 991–1003. https://doi.org/10.1038/nmat3776
[75] S. Ganta, H. Devalapally, A. Shahiwala, M. Amiji, A review of stimuli-responsive nanocarriers for drug and gene delivery, J. Control. Release. 126 (2008) 187–204. https://doi.org/10.1016/j.jconrel.2007.12.017
[76] H. Bi, J. Xue, H. Jiang, S. Gao, D. Yang, Y. Fang, K. Shi, Current developments in drug delivery with thermosensitive liposomes, Asian J. Pharm. Sci. (2018). https://doi.org/10.1016/J.AJPS.2018.07.006
[77] G. Bozzuto, A. Molinari, Liposomes as nanomedical devices, Int. J. Nanomedicine. 10 (2015) 975–999. https://doi.org/10.2147/IJN.S68861
[78] U. States, Thermosensitive Liposomes for Image-Guided Drug Delivery, 1st ed., Elsevier Inc., 2018. https://doi.org/10.1016/bs.acr.2018.04.004
[79] B. Kneidl, M. Peller, G. Winter, L.H. Lindner, M. Hossann, Thermosensitive liposomal drug delivery systems : State of the art review, Int J Nanomedicine. (2014) 4387–4398
[80] W. Rawicz, K.C. Olbrich, T. McIntosh, D. Needham, E. Evans, Effect of Chain Length and Unsaturation on Elasticity of Lipid Bilayers, Biophys. J. 79 (2000) 328–339. https://doi.org/10.1016/S0006-3495(00)76295-3
[81] J. Massiot, V. Rosilio, A. Makky, Photo-triggerable liposomal drug delivery systems: from simple porphyrin insertion in the lipid bilayer towards supramolecular assemblies of lipid–porphyrin conjugates, J. Mater. Chem. B. 7 (2019) 1805–1823. https://doi.org/10.1039/C9TB00015A
[82] S.J. Leung, M. Romanowski, Light-Activated Content Release from Liposomes, Theranostics. 2 (2012) 1020–1036. https://doi.org/10.7150/thno.4847
[83] B.S. Pattni, V. V. Chupin, V.P. Torchilin, New Developments in Liposomal Drug Delivery, Chem. Rev. 115 (2015) 10938–10966. https://doi.org/10.1021/acs.chemrev.5b00046
[84] A. Yavlovich, B. Smith, K. Gupta, R. Blumenthal, A. Puri, Light-sensitive lipid-based nanoparticles for drug delivery: design principles and future considerations for biological applications., Mol. Membr. Biol. 27 (2010) 364–81. https://doi.org/10.3109/09687688.2010.507788
[85] D. Conceição, D. Ferreira, L. Ferreira, D.S. Conceição, D.P. Ferreira, L.F.V. Ferreira, Photochemistry and Cytotoxicity Evaluation of Heptamethinecyanine Near Infrared (NIR) Dyes, Int. J. Mol. Sci. 14 (2013) 18557–18571. https://doi.org/10.3390/ijms140918557
[86] B. Chandra, S. Mallik, D.K. Srivastava, Design of photocleavable lipids and their application in liposomal “uncorking,” Chem. Commun. (2005) 3021. https://doi.org/10.1039/b503423j
[87] B. Chandra, R. Subramaniam, S. Mallik, D.K. Srivastava, Formulation of photocleavable liposomes and the mechanism of their content release, Org. Biomol. Chem. 4 (2006) 1730. https://doi.org/10.1039/b518359f
[88] S.L. Regen, A. Singh, G. Oehme, M. Singh, Polymerized phosphatidyl choline vesicles. Stabilized and controllable time-release carriers., Biochem. Biophys. Res. Commun. 101 (1981) 131–6. https://doi.org/10.1016/s0006-291x(81)80020-4
[89] A. Yavlovich, A. Singh, S. Tarasov, J. Capala, R. Blumenthal, A. Puri, Design of liposomes containing photopolymerizable phospholipids for triggered release of contents, J. Therm. Anal. Calorim. 98 (2009) 97–104. https://doi.org/10.1007/s10973-009-0228-8
[90] P. Shum, J.M. Kim, D.H. Thompson, Phototriggering of liposomal drug delivery systems., Adv. Drug Deliv. Rev. 53 (2001) 273–84
[91] Z. Li, Y. Wan, A.G. Kutateladze, Dithiane-based photolabile amphiphiles: toward photolabile liposomes1,2, Langmuir. 19 (2003) 6381–6391. https://doi.org/10.1021/LA034188M
[92] M. Mathiyazhakan, C. Wiraja, C. Xu, A Concise review of gold nanoparticles-based photo-responsive liposomes for controlled drug delivery, Nano-Micro Lett. 10 (2018) 10. https://doi.org/10.1007/s40820-017-0166-0
[93] H. Basoglu, M.D. Bilgin, M.M. Demir, Protoporphyrin IX-loaded magnetoliposomes as a potential drug delivery system for photodynamic therapy: Fabrication, characterization and in vitro study, Photodiagnosis Photodyn. Ther. 13 (2016) 81–90. https://doi.org/10.1016/j.pdpdt.2015.12.010
[94] A. Deshpande, M. Mohamed, S.B. Daftardar, M. Patel, S.H.S. Boddu, J. Nesamony, Solid Lipid nanoparticles in drug delivery: opportunities and challenges, emerg. nanotechnologies diagnostics, Drug Deliv. Med. Devices. (2017) 291–330. https://doi.org/10.1016/B978-0-323-42978-8.00012-7
[95] R.H. Müller, K. Mäder, S. Gohla, Solid lipid nanoparticles (SLN) for controlled drug delivery – A review of the state of the art, Eur. J. Pharm. Biopharm. 50 (2000) 161–177. https://doi.org/10.1016/S0939-6411(00)00087-4
[96] S. Mukherjee, S. Ray, R.S. Thakur, Solid lipid nanoparticles: a modern formulation approach in drug delivery system, Indian J. Pharm. Sci. 71 (2009) 349. https://doi.org/10.4103/0250-474X.57282
[97] N. Dudhipala, K. Veerabrahma, Pharmacokinetic and pharmacodynamic studies of nisoldipine-loaded solid lipid nanoparticles developed by central composite design, Drug Dev. Ind. Pharm. 41 (2015) 1968–1977. https://doi.org/10.3109/03639045.2015.1024685
[98] R.H. Müller, U. Alexiev, P. Sinambela, C.M. Keck, Nanostructured Lipid Carriers (NLC): The Second Generation of Solid Lipid Nanoparticles, in: Percutaneous Penetration Enhanc. Chem. Methods Penetration Enhanc., Springer Berlin Heidelberg, Berlin, Heidelberg, 2016: pp. 161–185. https://doi.org/10.1007/978-3-662-47862-2_11
[99] J.Y. Fang, C.L. Fang, C.H. Liu, Y.H. Su, Lipid nanoparticles as vehicles for topical psoralen delivery: Solid lipid nanoparticles (SLN) versus nanostructured lipid carriers (NLC), Eur. J. Pharm. Biopharm. 70 (2008) 633–640. https://doi.org/10.1016/J.EJPB.2008.05.008
[100] F. Tamjidi, M. Shahedi, J. Varshosaz, A. Nasirpour, Nanostructured lipid carriers (NLC): A potential delivery system for bioactive food molecules, Innov. Food Sci. Emerg. Technol. 19 (2013) 29–43. https://doi.org/10.1016/J.IFSET.2013.03.002
[101] B. Debelec-Butuner, M. Kotmakci, E. Oner, G. Ozduman, A.G. Kantarci, Nutlin3a-loaded nanoparticles show enhanced apoptotic activity on prostate cancer cells, Mol. Biotechnol. (2019). https://doi.org/10.1007/s12033-019-00178-2
[102] X. Liu, Q. Zhao, Long-term anesthetic analgesic effects: Comparison of tetracaine loaded polymeric nanoparticles, solid lipid nanoparticles, and nanostructured lipid carriers in vitro and in vivo, Biomed. Pharmacother. 117 (2019) 109057. https://doi.org/10.1016/j.biopha.2019.109057
[103] M. Üner, G. Yener, M. Ergüven, Design of colloidal drug carriers of celecoxib for use in treatment of breast cancer and leukemia, Mater. Sci. Eng. C. 103 (2019) 109874. https://doi.org/10.1016/j.msec.2019.109874
[104] M. Patel, V. Mundada, K. Sawant, Enhanced intestinal absorption of asenapine maleate by fabricating solid lipid nanoparticles using TPGS: Elucidation of transport mechanism, permeability across Caco-2 cell line and in vivo pharmacokinetic studies, Artif. Cells, Nanomedicine, Biotechnol. 47 (2019) 144–153. https://doi.org/10.1080/21691401.2018.1546186
[105] R. Bharadwaj, B.P. Sahu, J. Haloi, D. Laloo, P. Barooah, C. Keppen, M. Deka, S. Medhi, Combinatorial therapeutic approach for treatment of oral squamous cell carcinoma, Artif. Cells, Nanomedicine Biotechnol. 47 (2019) 572–585. https://doi.org/10.1080/21691401.2019.1573176
[106] R.H. Muller, C.M. Keck, Challenges and solutions for the delivery of biotech drugs – a review of drug nanocrystal technology and lipid nanoparticles, J. Biotechnol. 113 (2004) 151–170. https://doi.org/10.1016/J.JBIOTEC.2004.06.007
[107] P. Adhikari, P. Pal, A.K. Das, S. Ray, A. Bhattacharjee, B. Mazumder, Nano lipid-drug conjugate: An integrated review, Int. J. Pharm. 529 (2017) 629–641. https://doi.org/10.1016/J.IJPHARM.2017.07.039
[108] S. Verma, P. Utreja, Vesicular nanocarrier based treatment of skin fungal infections: Potential and emerging trends in nanoscale pharmacotherapy, Asian J. Pharm. Sci. 14 (2019) 117–129. https://doi.org/10.1016/j.ajps.2018.05.007
[109] H.A. Benson, Transfersomes for transdermal drug delivery, Expert Opin. Drug Deliv. 3 (2006) 727–737. https://doi.org/10.1517/17425247.3.6.727
[110] R. Rajan, S. Jose, V.P.B. Mukund, D.T. Vasudevan, Transferosomes – A vesicular transdermal delivery system for enhanced drug permeation, J. Adv. Pharm. Technol. Res. 2 (2011) 138–43. https://doi.org/10.4103/2231-4040.85524
[111] D.A.Y. Pawar, Transfersome: A novel technique which improves transdermal permeability, Asian J. Pharm. 10 (2016) 425–436. https://doi.org/10.22377/AJP.V10I04.875
[112] G. Cevc, G. Blume, Lipid vesicles penetrate into intact skin owing to the transdermal osmotic gradients and hydration force, Biochim. Biophys. Acta – Biomembr. 1104 (1992) 226–232. https://doi.org/10.1016/0005-2736(92)90154-E
[113] B. Bhasin, S.P. Patel, V.L.M. Road, An overview of transfersomal drug delivery bhavya bhasin and Vaishali Y. Londhe SVKM’S NMIMS , Shobhaben Pratapbhai Patel School of Pharmacy and Technology Management, Mumbai – 400056, Maharashtra, India., 9 (2018) 2175–2184. https://doi.org/10.13040/IJPSR.0975-8232.9(6).2175-84
[114] B. Bhasin, S.P. Patel, V.L.M. Road, An overview of transfersomal drug delivery, Int. J. Pharm. Sci. Res. 9 (2018) 2175–2184. https://doi.org/10.13040/IJPSR.0975-8232.9(6).2175-84
[115] A. Waheed, M. Aqil, A. Ahad, S.S. Imam, T. Moolakkadath, Z. Iqbal, A. Ali, AC SC, J. Drug Deliv. Sci. Technol. (2019). https://doi.org/10.1016/j.jddst.2019.05.019
[116] H. Song, H. Li, Y. Meng, Y. Zhang, N. Zhang, W. Zheng, Enhanced transdermal permeability and drug deposition of rheumatoid arthritis via sinomenine hydrochloride-loaded antioxidant surface transethosome, Int J Nanomedicine. 14 (2019) 3177–3188
[117] M.M. Omar, O.A. Hasan, A.M. El Sisi, Preparation and optimization of lidocaine transferosomal gel containing permeation enhancers : A promising approach for enhancement of skin permeation, Int J Nanomedicine. 14 (2019) 1551–1562
[118] P. Chaurasiya, E. Ganju, N. Upmanyu, S.K. Ray, P. Jain, Transfersomes: a novel technique for transdermal drug delivery, J. Drug Deliv. Ther. 9 (2019) 279–285. https://doi.org/10.22270/jddt.v9i1.2198
[119] A. Sankhyan, P. Pawar, Recent trends in niosome as vesicular drug delivery system, J. Appl. Pharm. Sci. 2 (2012) 20–32. https://doi.org/10.7324/JAPS.2012.2625
[120] I.F. Uchegbu, S.P. Vyas, Non-ionic surfactant based vesicles (niosomes) in drug delivery, Int. J. Pharm. 172 (1998) 33–70. https://doi.org/10.1016/S0378-5173(98)00169-0
[121] M.J. Choi, H.I. Maibach, Liposomes and niosomes as topical drug delivery systems, Skin Pharmacol. Physiol. 18 (2005) 209–219. https://doi.org/10.1159/000086666
[122] M. Gharbavi, J. Amani, H. Kheiri-Manjili, H. Danafar, A. Sharafi, Niosome: A promising nanocarrier for natural drug delivery through blood-brain barrier, Adv. Pharmacol. Sci. 2018 (2018). https://doi.org/10.1155/2018/6847971
[123] G.P. Kumar, P. Rajeshwarrao, Nonionic surfactant vesicular systems for effective drug delivery—an overview, Acta Pharm. Sin. B. 1 (2011) 208–219. https://doi.org/10.1016/J.APSB.2011.09.002
[124] T. Liu, R. Guo, Preparation of a highly stable niosome and its hydrotrope-solubilization action to drugs, Langmuir. 21-24 (2005) 11034-11039. https://doi.org/10.1021/LA051868B
[125] R. Rajera, K. Nagpal, S.K. Singh, D.N. Mishra, Niosomes: a controlled and novel drug delivery system., Biol. Pharm. Bull. 34 (2011) 945–53
[126] G. Amoabediny, F. Haghiralsadat, S. Naderinezhad, M.N. Helder, E. Akhoundi Kharanaghi, J. Mohammadnejad Arough, B. Zandieh-Doulabi, Overview of preparation methods of polymeric and lipid-based (niosome, solid lipid, liposome) nanoparticles: A comprehensive review, Int. J. Polym. Mater. Polym. Biomater. 67 (2018) 383–400. https://doi.org/10.1080/00914037.2017.1332623
[127] X. Ge, M. Wei, S. He, W.-E. Yuan, Advances of non-ionic surfactant vesicles (niosomes) and their application in drug delivery, Pharmaceutics. 11 (2019) 55. https://doi.org/10.3390/pharmaceutics11020055
[128] K.S. Yadav, R. Rajpurohit, S. Sharma, Glaucoma: Current treatment and impact of advanced drug delivery systems, Life Sci. 221 (2019) 362–376. https://doi.org/10.1016/j.lfs.2019.02.029
[129] R.G. Kerry, S. Malik, Y.T. Redda, S. Sahoo, J.K. Patra, S. Majhi, Nano-based approach to combat emerging viral (NIPAH virus) infection, Nanomedicine Nanotechnology Biol. Med. 18 (2019) 196–220. https://doi.org/10.1016/j.nano.2019.03.004
[130] A. Pal, S. Gupta, A. Jaiswal, A. Dube, S.P. Vyas, Development and evaluation of tripalmitin emulsomes for the treatment of experimental visceral leishmaniasis, J. Liposome Res. 22 (2012) 62–71. https://doi.org/10.3109/08982104.2011.592495
[131] N. Kossovsky, Biomolecular Delivery Using Coated Nanocrystalline Ceramics (Aquasomes), Nanotechnology. 626 (1996) 334–350. https://doi.org/10.1021/bk-1996-0622.ch023
[132] S. Banerjee, K.K. Sen, Aquasomes: A novel nanoparticulate drug carrier, J. Drug Deliv. Sci. Technol. 43 (2018) 446–452. https://doi.org/10.1016/J.JDDST.2017.11.011
[133] M.S. Umashankar, R.K. Sachdeva, M. Gulati, Aquasomes: A promising carrier for peptides and protein delivery, Nanomedicine Nanotechnology Biol. Med. 6 (2010) 419–426. https://doi.org/10.1016/J.NANO.2009.11.002
[134] S.S. Jain, P.S. Jagtap, N.M. Dand, K.R. Jadhav, V.J. Kadam, Aquasomes: A novel drug carrier, J. Appl. Pharm. Sci. 02 (2012) 184–192