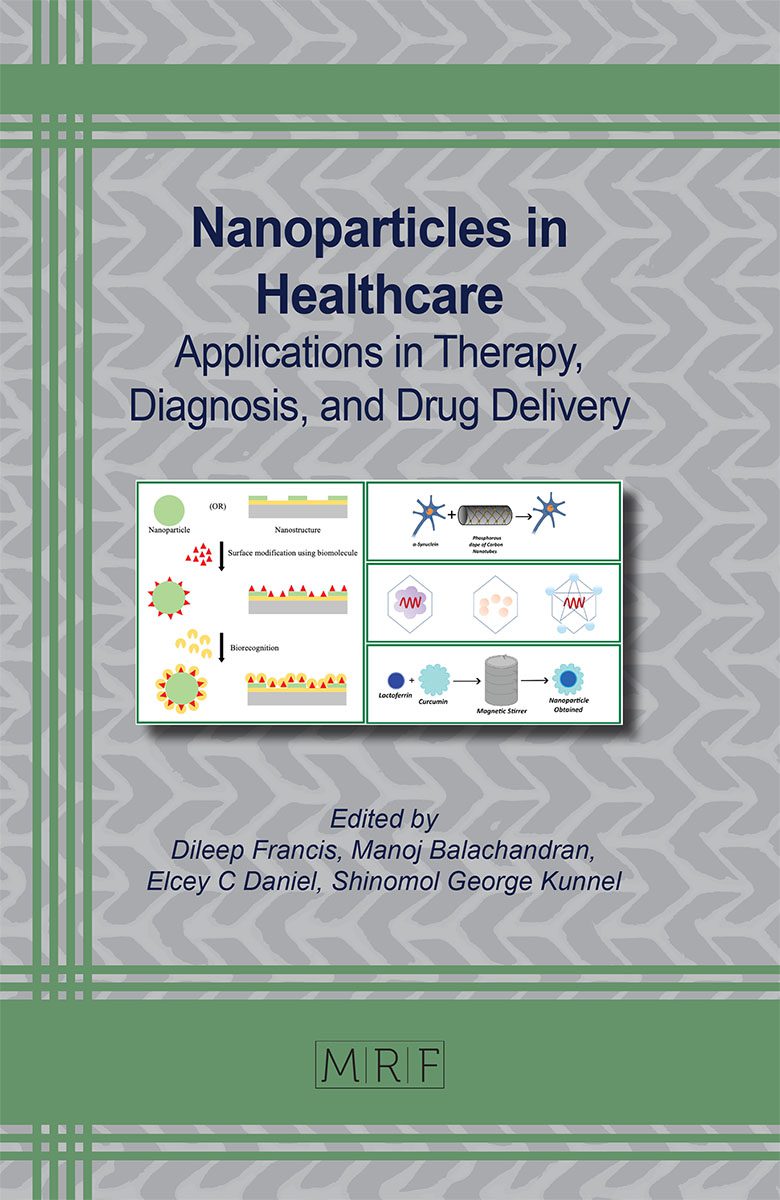
Applications of Nanoparticles in Bioimaging
Riya Thomas, Meera Varghese, Manoj Balachandran
Mounting stipulation for early identification and diagnosis of illnesses has constantly compelled the need for the development of non-invasive imaging techniques. These imaging methods work by exposing bodily tissues to a variety of energies, including magnetic fields, sound waves, radioactive chemicals, and high-energy radiations. Changes in the energy pattern that occur from these interactions are then used to create an image or picture. In order to provide more precise anatomical and functional information, contrast agents are utilized in imaging modalities to differentiate between normal tissue and pathological lesions. Compared to traditional contrast agents, nanoparticles (NPs) have attracted a lot of interest in the field of bioimaging due to their unique physicochemical traits and low toxicity profiles. Here in this chapter, we discuss the structure-related properties, benefits, and significant advancements of nanoparticle-based contrast agents used in the most popular biomedical imaging modalities.
Keywords
Biomedical Imaging, Nanoparticles, Contrast Agents, Tumor Detection
Published online 2/10/2024, 32 pages
Citation: Riya Thomas, Meera Varghese, Manoj Balachandran, Applications of Nanoparticles in Bioimaging, Materials Research Foundations, Vol. 160, pp 113-144, 2024
DOI: https://doi.org/10.21741/9781644902974-5
Part of the book on Nanoparticles in Healthcare
References
[1] R. Rani, K. Sethi, and G. Singh, “Nanomaterials and Their Applications in Bioimaging,” Nanotechnol. Life Sci., pp. 429-450, 2019. https://doi.org/10.1007/978-3-030-16379-2_15
[2] R. Thomas, J. Unnikrishnan, A. V. Nair, E. C. Daniel, and M. Balachandran, “Antibacterial performance of GO-Ag nanocomposite prepared via ecologically safe protocols,” Appl. Nanosci., vol. 10, no. 11, pp. 4207-4219, 2020. https://doi.org/10.1007/s13204-020-01539-z
[3] A. V. Ramya and M. Balachandran, “Valorization of agro-industrial fruit peel waste to fluorescent nanocarbon sensor: Ultrasensitive detection of potentially hazardous tropane alkaloid,” Front. Environ. Sci. Eng., vol. 16, no. 3, p. 27, 2021. https://doi.org/10.1007/s11783-021-1461-z
[4] A. N. Mohan and S. Panicker, “Facile synthesis of graphene-tin oxide nanocomposite derived from agricultural waste for enhanced antibacterial activity against Pseudomonas aeruginosa,” Sci. Rep., vol. 9, no. 1, pp. 1-12, 2019. https://doi.org/10.1038/s41598-019-40916-9
[5] S. S. Mughal, “DIAGNOSIS AND TREATMENT OF DISEASES BY USING METALLIC NANOPARTICLES-A REVIEW,” Authorea Prepr., 2022. https://doi.org/10.22541/au.166401168.84305772/v1
[6] N. Aslan, B. Ceylan, M. M. Koç, and F. Findik, “Metallic nanoparticles as X-Ray computed tomography (CT) contrast agents: A review,” J. Mol. Struct., vol. 1219, p. 128599, 2020. https://doi.org/10.1016/j.molstruc.2020.128599
[7] Z. Wei et al., “Rare-earth based materials: an effective toolbox for brain imaging, therapy, monitoring and neuromodulation,” Light Sci. Appl., vol. 11, no. 1, p. 175, 2022. https://doi.org/10.1038/s41377-022-00922-5
[8] X. Zhu et al., “High‐fidelity NIR‐II multiplexed lifetime bioimaging with bright double interfaced lanthanide nanoparticles,” Angew. Chemie, vol. 133, no. 44, pp. 23737-23743, 2021. https://doi.org/10.1002/ange.202108124
[9] G. Zhu et al., “GdVO4: Eu3+, Bi3+ nanoparticles as a contrast agent for MRI and luminescence bioimaging,” ACS omega, vol. 4, no. 14, pp. 15806-15814, 2019. https://doi.org/10.1021/acsomega.9b00444
[10] R. De Matos et al., “Gd3+-Functionalized Lithium Niobate Nanoparticles for Dual Multiphoton and Magnetic Resonance Bioimaging,” ACS Appl. Nano Mater., vol. 5, no. 2, pp. 2912-2922, 2022. https://doi.org/10.1021/acsanm.2c00127
[11] P. Araichimani et al., “Rare-earth ions integrated silica nanoparticles derived from rice husk via microwave-assisted combustion method for bioimaging applications,” Ceram. Int., vol. 46, no. 11, pp. 18366-18372, 2020. https://doi.org/10.1016/j.ceramint.2020.04.125
[12] T. Jia et al., “Mesoporous cerium oxide-coated upconversion nanoparticles for tumor-responsive chemo-photodynamic therapy and bioimaging,” Chem. Sci., vol. 10, no. 37, pp. 8618-8633, 2019. https://doi.org/10.1039/C9SC01615E
[13] X. Shan et al., “Polypyrrole-based double rare earth hybrid nanoparticles for multimodal imaging and photothermal therapy,” J. Mater. Chem. B, vol. 8, no. 3, pp. 426-437, 2020. https://doi.org/10.1039/C9TB02254F
[14] F. Ren et al., “NIR‐II Fluorescence imaging for cerebrovascular diseases,” View, vol. 2, no. 6, p. 20200128, 2021. https://doi.org/10.1002/VIW.20200128
[15] D. Song, M. Zhu, S. Chi, L. Xia, Z. Li, and Z. Liu, “Sensitizing the luminescence of lanthanide-doped nanoparticles over 1500 nm for high-contrast and deep imaging of brain injury,” Anal. Chem., vol. 93, no. 22, pp. 7949-7957, 2021. https://doi.org/10.1021/acs.analchem.1c00731
[16] Q. Wang, T. Liang, J. Wu, Z. Li, and Z. Liu, “Dye-sensitized rare earth-doped nanoparticles with boosted NIR-IIb emission for dynamic imaging of vascular network-related disorders,” ACS Appl. Mater. Interfaces, vol. 13, no. 25, pp. 29303-29312, 2021. https://doi.org/10.1021/acsami.1c04612
[17] Y. C. Dong et al., “Ytterbium Nanoparticle Contrast Agents for Conventional and Spectral Photon-Counting CT and Their Applications for Hydrogel Imaging,” ACS Appl. Mater. Interfaces, vol. 14, no. 34, pp. 39274-39284, 2022. https://doi.org/10.1021/acsami.2c12354
[18] M. Chang et al., “Enhanced photoconversion performance of NdVO4/Au nanocrystals for photothermal/photoacoustic imaging guided and near infrared light-triggered anticancer phototherapy,” Acta Biomater., vol. 99, pp. 295-306, 2019. https://doi.org/10.1016/j.actbio.2019.08.026
[19] Z. Yu et al., “Achieving effective multimodal imaging with rare-earth ion-doped CaF2 nanoparticles,” Pharmaceutics, vol. 14, no. 4, p. 840, 2022. https://doi.org/10.3390/pharmaceutics14040840
[20] X. Shi, K. Gao, G. Zhang, W. Zhang, X. Yang, and R. Gao, “Signal Amplification Pretargeted PET/Fluorescence Imaging Based on Human Serum Albumin-Encapsulated GdF3 Nanoparticles for Diagnosis of Ovarian Cancer,” ACS Biomater. Sci. Eng., vol. 8, no. 11, pp. 4956-4964, 2022. https://doi.org/10.1021/acsbiomaterials.2c00374
[21] J. Cheng et al., “AgBiS2 nanoparticles with synergistic photodynamic and bioimaging properties for enhanced malignant tumor phototherapy,” Mater. Sci. Eng. C, vol. 107, p. 110324, 2020. https://doi.org/10.1016/j.msec.2019.110324
[22] Q. Cheng et al., “Supramolecular Tropism Driven Aggregation of Nanoparticles In Situ for Tumor‐Specific Bioimaging and Photothermal Therapy,” Small, vol. 17, no. 43, p. 2101332, 2021. https://doi.org/10.1002/smll.202101332
[23] D. S. Dumani, I.-C. Sun, and S. Y. Emelianov, “Ultrasound-guided immunofunctional photoacoustic imaging for diagnosis of lymph node metastases,” Nanoscale, vol. 11, no. 24, pp. 11649-11659, 2019. https://doi.org/10.1039/C9NR02920F
[24] O. J. Estudiante-Mariquez, A. Rodríguez-Galván, D. Ramírez-Hernández, F. F. Contreras-Torres, and L. A. Medina, “Technetium-radiolabeled mannose-functionalized gold nanoparticles as nanoprobes for sentinel lymph node detection,” Molecules, vol. 25, no. 8, p. 1982, 2020. https://doi.org/10.3390/molecules25081982
[25] Y. Li, D. Xiao, S. Li, Z. Chen, S. Liu, and J. Li, “Silver@ quercetin nanoparticles with aggregation-induced emission for bioimaging in vitro and in vivo,” Int. J. Mol. Sci., vol. 23, no. 13, p. 7413, 2022. https://doi.org/10.3390/ijms23137413
[26] M. Bouché et al., “Activatable hybrid polyphosphazene-AuNP nanoprobe for ROS detection by bimodal PA/CT imaging,” ACS Appl. Mater. Interfaces, vol. 11, no. 32, pp. 28648-28656, 2019. https://doi.org/10.1021/acsami.9b08386
[27] M. Lyu, D. Zhu, Y. Duo, Y. Li, and H. Quan, “Bimetallic nanodots for tri-modal CT/MRI/PA imaging and hypoxia-resistant thermoradiotherapy in the NIR-II biological windows,” Biomaterials, vol. 233, p. 119656, 2020. https://doi.org/10.1016/j.biomaterials.2019.119656
[28] D. Li et al., “Metal-organic nanostructure based on TixOy/Ruthenium reaction Units: For CT/MR Imaging-Guided X-ray induced dynamic therapy,” Chem. Eng. J., vol. 417, p. 129262, 2021. https://doi.org/10.1016/j.cej.2021.129262
[29] S. D. Anderson, V. V Gwenin, and C. D. Gwenin, “Magnetic functionalized nanoparticles for biomedical, drug delivery and imaging applications,” Nanoscale Res. Lett., vol. 14, no. 1, pp. 1-16, 2019. https://doi.org/10.1186/s11671-019-3019-6
[30] S. Carregal‐Romero et al., “Ultrasmall manganese ferrites for in vivo catalase mimicking activity and multimodal bioimaging,” Small, vol. 18, no. 16, p. 2106570, 2022. https://doi.org/10.1002/smll.202106570
[31] S. Gull, F. Ahmad, W. Wu, and W. Li, “Manganese-doped cesium iodide nanoparticles for multi-model bioimaging,” Mater. Lett., vol. 256, p. 126630, 2019. https://doi.org/10.1016/j.matlet.2019.126630
[32] N. J. Hobson et al., “Clustering superparamagnetic iron oxide nanoparticles produces organ-targeted high-contrast magnetic resonance images,” Nanomedicine, vol. 14, no. 9, pp. 1135-1152, 2019. https://doi.org/10.2217/nnm-2018-0370
[33] V. Pandey, T. Haider, P. Agrawal, S. Soni, and V. Soni, “Advances in Natural Polymeric Nanoparticles for the Drug Delivery,” in Advances in Drug Delivery Methods, IntechOpen, 2022. https://doi.org/10.5772/intechopen.107513
[34] I. Parveen, M. I. Mahmud, and R. A. Khan, “Biodegradable Natural Polymers for Biomedical Applications,” Guigoz. Sci. Rev., vol. 5, no. 3, pp. 67-80, 2019. https://doi.org/10.32861/sr.53.67.80
[35] B. Patra, A. K. Mishra, and R. S. Verma, “Label-free serum albumin nanoparticles for bioimaging and Trojan horse-like drug delivery,” J. Sci. Adv. Mater. Devices, vol. 7, no. 1, p. 100406, 2022. https://doi.org/10.1016/j.jsamd.2021.100406
[36] Q. Wang, J. Fan, Y. Zhou, and S. Xu, “Development of a human serum albumin structure-based fluorescent probe for bioimaging in living cells,” Spectrochim. Acta Part A Mol. Biomol. Spectrosc., vol. 269, p. 120769, 2022. https://doi.org/10.1016/j.saa.2021.120769
[37] L. L. Radford et al., “New 55Co-labeled albumin-binding folate derivatives as potential PET agents for folate receptor imaging,” Pharmaceuticals, vol. 12, no. 4, p. 166, 2019. https://doi.org/10.3390/ph12040166
[38] D. Gao et al., “Albumin-consolidated AIEgens for boosting glioma and cerebrovascular NIR-II fluorescence imaging,” ACS Appl. Mater. Interfaces, vol. 15, no. 1, pp. 3-13, 2022. https://doi.org/10.1021/acsami.1c22700
[39] Y. Zhang, Y. Wan, Y. Chen, N. T. Blum, J. Lin, and P. Huang, “Ultrasound-enhanced chemo-photodynamic combination therapy by using albumin ‘nanoglue’-based nanotheranostics,” ACS Nano, vol. 14, no. 5, pp. 5560-5569, 2020. https://doi.org/10.1021/acsnano.9b09827
[40] D. Li, T. Zhang, C. Min, H. Huang, D. Tan, and W. Gu, “Biodegradable theranostic nanoplatforms of albumin-biomineralized nanocomposites modified hollow mesoporous organosilica for photoacoustic imaging guided tumor synergistic therapy,” Chem. Eng. J., vol. 388, p. 124253, 2020. https://doi.org/10.1016/j.cej.2020.124253
[41] Z. Yang et al., “Albumin-based nanotheranostic probe with hypoxia alleviating potentiates synchronous multimodal imaging and phototherapy for glioma,” ACS Nano, vol. 14, no. 5, pp. 6191-6212, 2020. https://doi.org/10.1021/acsnano.0c02249
[42] A. Baki, A. Remmo, N. Löwa, F. Wiekhorst, and R. Bleul, “Albumin-coated single-core iron oxide nanoparticles for enhanced molecular magnetic imaging (Mri/mpi),” Int. J. Mol. Sci., vol. 22, no. 12, p. 6235, 2021. https://doi.org/10.3390/ijms22126235
[43] N. El‐Sayed, V. Trouillet, A. Clasen, G. Jung, K. Hollemeyer, and M. Schneider, “NIR‐Emitting Gold Nanoclusters-Modified Gelatin Nanoparticles as a Bioimaging Agent in Tissue,” Adv. Healthc. Mater., vol. 8, no. 24, p. 1900993, 2019. https://doi.org/10.1002/adhm.201900993
[44] Y. Xue et al., “Rhodamine Conjugated Gelatin Methacryloyl Nanoparticles for Stable Cell Imaging,” ACS Appl. Bio Mater., vol. 3, no. 10, pp. 6908-6918, 2020. https://doi.org/10.1021/acsabm.0c00802
[45] S. Paul et al., “Hydrothermal synthesis of gelatin quantum dots for high-performance biological imaging applications,” J. Photochem. Photobiol. B Biol., vol. 212, p. 112014, 2020. https://doi.org/10.1016/j.jphotobiol.2020.112014
[46] A. Kimura et al., “Ultra-small size gelatin nanogel as a blood brain barrier impermeable contrast agent for magnetic resonance imaging,” Acta Biomater., vol. 125, pp. 290-299, 2021. https://doi.org/10.1016/j.actbio.2021.02.016
[47] R. Yang et al., “Biomineralization-inspired crystallization of manganese oxide on silk fibroin nanoparticles for in vivo MR/fluorescence imaging-assisted tri-modal therapy of cancer,” Theranostics, vol. 9, no. 21, p. 6314, 2019. https://doi.org/10.7150/thno.36252
[48] R. Ma et al., “Clinical indocyanine green-based silk fibroin theranostic nanoprobes for in vivo NIR-I/II fluorescence imaging of cervical diseases,” Nanomedicine Nanotechnology, Biol. Med., vol. 47, p. 102615, 2023. https://doi.org/10.1016/j.nano.2022.102615
[49] Y. Wang et al., “In vivo photoacoustic/single-photon emission computed tomography imaging for dynamic monitoring of aggregation-enhanced photothermal nanoagents,” Anal. Chem., vol. 91, no. 3, pp. 2128-2134, 2019. https://doi.org/10.1021/acs.analchem.8b04585
[50] M. Salarian et al., “Precision detection of liver metastasis by collagen-targeted protein MRI contrast agent,” Biomaterials, vol. 224, p. 119478, 2019. https://doi.org/10.1016/j.biomaterials.2019.119478
[51] X. Zhou, L. Guo, D. Shi, S. Duan, and J. Li, “Biocompatible chitosan nanobubbles for ultrasound-mediated targeted delivery of doxorubicin,” Nanoscale Res. Lett., vol. 14, pp. 1-9, 2019. https://doi.org/10.1186/s11671-019-2853-x
[52] H. Xiao et al., “Preparation of fluorescent nanoparticles based on broken-rice starch for live-cell imaging,” Int. J. Biol. Macromol., vol. 217, pp. 88-95, 2022. https://doi.org/10.1016/j.ijbiomac.2022.06.205
[53] W. Zhou et al., “Iodine‐rich semiconducting polymer nanoparticles for CT/Fluorescence dual‐modal imaging‐guided enhanced photodynamic therapy,” Small, vol. 16, no. 5, p. 1905641, 2020. https://doi.org/10.1002/smll.201905641
[54] Y. Yang et al., “A 1064 nm excitable semiconducting polymer nanoparticle for photoacoustic imaging of gliomas,” Nanoscale, vol. 11, no. 16, pp. 7754-7760, 2019. https://doi.org/10.1039/C9NR00552H
[55] M. Liu, Z. Zhang, Y. Yang, and Y. Chan, “Polymethine‐Based Semiconducting Polymer Dots with Narrow‐Band Emission and Absorption/Emission Maxima at NIR‐II for Bioimaging,” Angew. Chemie Int. Ed., vol. 60, no. 2, pp. 983-989, 2021. https://doi.org/10.1002/anie.202011914
[56] B. Guo et al., “High‐resolution 3D NIR‐II photoacoustic imaging of cerebral and tumor vasculatures using conjugated polymer nanoparticles as contrast agent,” Adv. Mater., vol. 31, no. 25, p. 1808355, 2019. https://doi.org/10.1002/adma.201808355
[57] Y. Liu et al., “Fluorination enhances NIR‐II fluorescence of polymer dots for quantitative brain tumor imaging,” Angew. Chemie, vol. 132, no. 47, pp. 21235-21243, 2020. https://doi.org/10.1002/ange.202007886
[58] J. Zhao et al., “H 2 O 2-sensitive nanoscale coordination polymers for photoacoustic tumors imaging via in vivo chromogenic assay.,” J. Innov. Opt. Health Sci., vol. 15, no. 5, 2022. https://doi.org/10.1142/S1793545822500262
[59] X. Hu et al., “Gadolinium-chelated conjugated polymer-based nanotheranostics for photoacoustic/magnetic resonance/NIR-II fluorescence imaging-guided cancer photothermal therapy,” Theranostics, vol. 9, no. 14, p. 4168, 2019. https://doi.org/10.7150/thno.34390
[60] Z. Chen et al., “The advances of carbon nanotubes in cancer diagnostics and therapeutics,” J. Nanomater., vol. 2017, 2017. https://doi.org/10.1155/2017/3418932
[61] A. De La Zerda et al., “Carbon nanotubes as photoacoustic molecular imaging agents in living mice,” Nat. Nanotechnol., vol. 3, no. 9, pp. 557-562, 2008. https://doi.org/10.1038/nnano.2008.231
[62] M. Pramanik, M. Swierczewska, D. Green, B. Sitharaman, and L. V Wang, “Single-walled carbon nanotubes as a multimodal-thermoacoustic and photoacoustic-contrast agent,” J. Biomed. Opt., vol. 14, no. 3, p. 34018, 2009. https://doi.org/10.1117/1.3147407
[63] L. Xie et al., “Functional long circulating single walled carbon nanotubes for fluorescent/photoacoustic imaging-guided enhanced phototherapy,” Biomaterials, vol. 103, pp. 219-228, 2016. https://doi.org/10.1016/j.biomaterials.2016.06.058
[64] H. Gong, R. Peng, and Z. Liu, “Carbon nanotubes for biomedical imaging: the recent advances,” Adv. Drug Deliv. Rev., vol. 65, no. 15, pp. 1951-1963, 2013. https://doi.org/10.1016/j.addr.2013.10.002
[65] Z. Liu et al., “Multiplexed five-color molecular imaging of cancer cells and tumor tissues with carbon nanotube Raman tags in the near-infrared,” Nano Res., vol. 3, pp. 222-233, 2010. https://doi.org/10.1007/s12274-010-1025-1
[66] X. Wang, C. Wang, L. Cheng, S.-T. Lee, and Z. Liu, “Noble metal coated single-walled carbon nanotubes for applications in surface enhanced Raman scattering imaging and photothermal therapy,” J. Am. Chem. Soc., vol. 134, no. 17, pp. 7414-7422, 2012. https://doi.org/10.1021/ja300140c
[67] A. Jorio, M. A. Pimenta, A. G. Souza Filho, R. Saito, G. Dresselhaus, and M. S. Dresselhaus, “Characterizing carbon nanotube samples with resonance Raman scattering,” New J. Phys., vol. 5, no. 1, p. 139, 2003. https://doi.org/10.1088/1367-2630/5/1/139
[68] J. T. Robinson, G. Hong, Y. Liang, B. Zhang, O. K. Yaghi, and H. Dai, “In vivo fluorescence imaging in the second near-infrared window with long circulating carbon nanotubes capable of ultrahigh tumor uptake,” J. Am. Chem. Soc., vol. 134, no. 25, pp. 10664-10669, 2012. https://doi.org/10.1021/ja303737a
[69] K. Welsher et al., “A route to brightly fluorescent carbon nanotubes for near-infrared imaging in mice,” Nat. Nanotechnol., vol. 4, no. 11, pp. 773-780, 2009. https://doi.org/10.1038/nnano.2009.294
[70] S.-T. Yang et al., “Carbon dots as nontoxic and high-performance fluorescence imaging agents,” J. Phys. Chem. C, vol. 113, no. 42, pp. 18110-18114, 2009. https://doi.org/10.1021/jp9085969
[71] Y. Song, W. Shi, W. Chen, X. Li, and H. Ma, “Fluorescent carbon nanodots conjugated with folic acid for distinguishing folate-receptor-positive cancer cells from normal cells,” J. Mater. Chem., vol. 22, no. 25, pp. 12568-12573, 2012. https://doi.org/10.1039/c2jm31582c
[72] N. Parvin and T. K. Mandal, “Dually emissive P, N-co-doped carbon dots for fluorescent and photoacoustic tissue imaging in living mice,” Microchim. Acta, vol. 184, pp. 1117-1125, 2017. https://doi.org/10.1007/s00604-017-2108-4
[73] G. Xu et al., “In vivo tumor photoacoustic imaging and photothermal therapy based on supra‐(carbon nanodots),” Adv. Healthc. Mater., vol. 8, no. 2, p. 1800995, 2019. https://doi.org/10.1002/adhm.201800995
[74] S. Sun et al., “Ce6-modified carbon dots for multimodal-imaging-guided and single-NIR-laser-triggered photothermal/photodynamic synergistic cancer therapy by reduced irradiation power,” ACS Appl. Mater. Interfaces, vol. 11, no. 6, pp. 5791-5803, 2019. https://doi.org/10.1021/acsami.8b19042
[75] D. Bouzas‐Ramos, J. Cigales Canga, J. C. Mayo, R. M. Sainz, J. Ruiz Encinar, and J. M. Costa‐Fernandez, “Carbon quantum dots codoped with nitrogen and lanthanides for multimodal imaging,” Adv. Funct. Mater., vol. 29, no. 38, p. 1903884, 2019. https://doi.org/10.1002/adfm.201903884
[76] X. Zhao et al., “A magnetofluorescent boron-doped carbon dots as a metal-free bimodal probe,” Talanta, vol. 200, pp. 9-14, 2019. https://doi.org/10.1016/j.talanta.2019.03.022
[77] J. Zhang et al., “Phosphorescent Carbon Dots for Highly Efficient Oxygen Photosensitization and as Photo-oxidative Nanozymes,” ACS Appl. Mater. Interfaces, vol. 10, pp. 40808-40814, 2018, doi: 10.1021/acsami.8b15318. https://doi.org/10.1021/acsami.8b15318
[78] Z. Liu, Z. Guo, H. Zhong, X. Qin, M. Wan, and B. Yang, “Graphene oxide based surface-enhanced Raman scattering probes for cancer cell imaging,” Phys. Chem. Chem. Phys., vol. 15, no. 8, pp. 2961-2966, 2013. https://doi.org/10.1039/c2cp43715e
[79] Y. Chen, T. Liu, P. Chen, P. Chang, and S. Chen, “A high‐sensitivity and low‐power theranostic nanosystem for cell SERS imaging and selectively photothermal therapy using anti‐EGFR‐conjugated reduced graphene oxide/mesoporous silica/AuNPs nanosheets,” Small, vol. 12, no. 11, pp. 1458-1468, 2016. https://doi.org/10.1002/smll.201502917
[80] Y. Esmaeili, E. Bidram, A. Zarrabi, A. Amini, and C. Cheng, “Graphene oxide and its derivatives as promising In-vitro bio-imaging platforms,” Sci. Rep., vol. 10, no. 1, pp. 1-13, 2020. https://doi.org/10.1038/s41598-020-75090-w
[81] P. S. Wate et al., “Cellular imaging using biocompatible dendrimer-functionalized graphene oxide-based fluorescent probe anchored with magnetic nanoparticles,” Nanotechnology, vol. 23, no. 41, p. 415101, 2012. https://doi.org/10.1088/0957-4484/23/41/415101
[82] P. Huang et al., “Surface functionalization of chemically reduced graphene oxide for targeted photodynamic therapy,” J. Biomed. Nanotechnol., vol. 11, no. 1, pp. 117-125, 2015. https://doi.org/10.1166/jbn.2015.2055
[83] R. Thomas and M. Balachandran, “Doable production of highly fluorescent, heteroatom-doped graphene material from fuel coke for cellular bioimaging: An eco-sustainable cradle-to-gate approach,” J. Clean. Prod., vol. 383, p. 135541, 2023. https://doi.org/10.1016/j.jclepro.2022.135541
[84] G. Lalwani, X. Cai, L. Nie, L. V. Wang, and B. Sitharaman, “Graphene-based contrast agents for photoacoustic and thermoacoustic tomography,” Photoacoustics, vol. 1, no. 3-4, pp. 62-67, 2013, doi: 10.1016/j.pacs.2013.10.001. https://doi.org/10.1016/j.pacs.2013.10.001
[85] S. Lee and S. Y. Kim, “Gold nanorod/reduced graphene oxide composite nanocarriers for near-infrared-induced cancer therapy and photoacoustic imaging,” ACS Appl. Nano Mater., vol. 4, no. 11, pp. 11849-11860, 2021. https://doi.org/10.1021/acsanm.1c02419
[86] J. Chen et al., “Indocyanine green loaded reduced graphene oxide for in vivo photoacoustic/fluorescence dual-modality tumor imaging,” Nanoscale Res. Lett., vol. 11, pp. 1-11, 2016. https://doi.org/10.1186/s11671-016-1288-x
[87] H. W. Yang et al., “Gadolinium-functionalized nanographene oxide for combined drug and microRNA delivery and magnetic resonance imaging,” Biomaterials, vol. 35, no. 24, pp. 6534-6542, 2014, doi: 10.1016/j.biomaterials.2014.04.057. https://doi.org/10.1016/j.biomaterials.2014.04.057
[88] K. Yang, L. Feng, X. Shi, and Z. Liu, “Nano-graphene in biomedicine: theranostic applications,” Chem. Soc. Rev., vol. 42, no. 2, pp. 530-547, 2013. https://doi.org/10.1039/C2CS35342C
[89] K. Yang et al., “Multimodal imaging guided photothermal therapy using functionalized graphene nanosheets anchored with magnetic nanoparticles,” Adv. Mater., vol. 24, no. 14, pp. 1868-1872, 2012. https://doi.org/10.1002/adma.201104964
[90] M. R. Younis, G. He, J. Lin, and P. Huang, “Recent advances on graphene quantum dots for bioimaging applications,” Front. Chem., vol. 8, p. 424, 2020. https://doi.org/10.3389/fchem.2020.00424
[91] L. Wang et al., “Ultrastable amine, sulfo cofunctionalized graphene quantum dots with high two-photon fluorescence for cellular imaging,” ACS Sustain. Chem. Eng., vol. 6, no. 4, pp. 4711-4716, 2018. https://doi.org/10.1021/acssuschemeng.7b03797
[92] T. Gao et al., “Red, yellow, and blue luminescence by graphene quantum dots: syntheses, mechanism, and cellular imaging,” ACS Appl. Mater. Interfaces, vol. 9, no. 29, pp. 24846-24856, 2017. https://doi.org/10.1021/acsami.7b05569
[93] H. Wang et al., “Nitrogen and boron dual-doped graphene quantum dots for near-infrared second window imaging and photothermal therapy,” Appl. Mater. today, vol. 14, pp. 108-117, 2019. https://doi.org/10.1016/j.apmt.2018.11.011
[94] M. C. Biswas, M. T. Islam, P. K. Nandy, and M. M. Hossain, “Graphene quantum dots (GQDs) for bioimaging and drug delivery applications: a review,” ACS Mater. Lett., vol. 3, no. 6, pp. 889-911, 2021. https://doi.org/10.1021/acsmaterialslett.0c00550
[95] F. H. Wang, K. Bae, Z. W. Huang, and J. M. Xue, “Two-photon graphene quantum dot modified Gd 2 O 3 nanocomposites as a dual-mode MRI contrast agent and cell labelling agent,” Nanoscale, vol. 10, no. 12, pp. 5642-5649, 2018. https://doi.org/10.1039/C7NR08068A
[96] H. Wang et al., “Paramagnetic properties of metal-free boron-doped graphene quantum dots and their application for safe magnetic resonance imaging,” Adv. Mater., vol. 29, no. 11, 2017. https://doi.org/10.1002/adma.201605416
[97] S. Badrigilan, B. Shaabani, N. G. Aghaji, and A. Mesbahi, “Graphene quantum dots-coated bismuth nanoparticles for improved CT imaging and photothermal performance,” Int. J. Nanosci., vol. 19, no. 01, p. 1850043, 2020. https://doi.org/10.1142/S0219581X18500436
[98] Y. Xuan et al., “Targeting N-doped graphene quantum dot with high photothermal conversion efficiency for dual-mode imaging and therapy in vitro,” Nanotechnology, vol. 29, no. 35, p. 355101, 2018. https://doi.org/10.1088/1361-6528/aacad0
[99] S. K. Nune, P. Gunda, P. K. Thallapally, Y.-Y. Lin, M. Laird Forrest, and C. J. Berkland, “Nanoparticles for biomedical imaging,” Expert Opin. Drug Deliv., vol. 6, no. 11, pp. 1175-1194, 2009. https://doi.org/10.1517/17425240903229031
[100] S. Mosleh-Shirazi et al., “Nanotechnology Advances in the Detection and Treatment of Cancer: An Overview,” Nanotheranostics, vol. 6, no. 4, pp. 400-423, 2022, doi: 10.7150/ntno.74613. https://doi.org/10.7150/ntno.74613
[101] C.-J. Wen, C. T. Sung, I. A. Aljuffali, Y.-J. Huang, and J.-Y. Fang, “Nanocomposite liposomes containing quantum dots and anticancer drugs for bioimaging and therapeutic delivery: a comparison of cationic, PEGylated and deformable liposomes,” Nanotechnology, vol. 24, no. 32, p. 325101, 2013. https://doi.org/10.1088/0957-4484/24/32/325101
[102] S. Dong, J. D. W. Teo, L. Y. Chan, C.-L. K. Lee, and K. Sou, “Far-red fluorescent liposomes for folate receptor-targeted bioimaging,” ACS Appl. Nano Mater., vol. 1, no. 3, pp. 1009-1013, 2018. https://doi.org/10.1021/acsanm.8b00084
[103] N. Kostevšek et al., “Magneto-liposomes as MRI contrast agents: A systematic study of different liposomal formulations,” Nanomaterials, vol. 10, no. 5, p. 889, 2020. https://doi.org/10.3390/nano10050889
[104] R. S. Garcia Ribeiro et al., “Targeting tumor cells and neovascularization using RGD-functionalized magnetoliposomes,” Int. J. Nanomedicine, pp. 5911-5924, 2019. https://doi.org/10.2147/IJN.S214041
[105] C. T. Badea et al., “Computed tomography imaging of primary lung cancer in mice using a liposomal-iodinated contrast agent,” PLoS One, vol. 7, no. 4, p. e34496, 2012. https://doi.org/10.1371/journal.pone.0034496
[106] M. Silindir et al., “Nanosized multifunctional liposomes for tumor diagnosis and molecular imaging by SPECT/CT,” J. Liposome Res., vol. 23, no. 1, pp. 20-27, 2013. https://doi.org/10.3109/08982104.2012.722107
[107] S. Valetti, S. Mura, B. Stella, and P. Couvreur, “Rational design for multifunctional non-liposomal lipid-based nanocarriers for cancer management: theory to practice,” J. Nanobiotechnology, vol. 11, no. 1, pp. 1-17, 2013. https://doi.org/10.1186/1477-3155-11-S1-S6
[108] A.-K. Kirchherr, A. Briel, and K. Mäder, “Stabilization of indocyanine green by encapsulation within micellar systems,” Mol. Pharm., vol. 6, no. 2, pp. 480-491, 2009. https://doi.org/10.1021/mp8001649
[109] X. Zheng, D. Xing, F. Zhou, B. Wu, and W. R. Chen, “Indocyanine green-containing nanostructure as near infrared dual-functional targeting probes for optical imaging and photothermal therapy,” Mol. Pharm., vol. 8, no. 2, pp. 447-456, 2011. https://doi.org/10.1021/mp100301t
[110] F. Ducongé et al., “Fluorine-18-labeled phospholipid quantum dot micelles for in vivo multimodal imaging from whole body to cellular scales,” Bioconjug. Chem., vol. 19, no. 9, pp. 1921-1926, 2008. https://doi.org/10.1021/bc800179j
[111] D. Zhang et al., “Lipid micelles packaged with semiconducting polymer dots as simultaneous MRI/photoacoustic imaging and photodynamic/photothermal dual-modal therapeutic agents for liver cancer,” J. Mater. Chem. B, vol. 4, no. 4, pp. 589-599, 2016. https://doi.org/10.1039/C5TB01827G
[112] W. Li et al., “α-Lipoic acid stabilized DTX/IR780 micelles for photoacoustic/fluorescence imaging guided photothermal therapy/chemotherapy of breast cancer,” Biomater. Sci., vol. 6, no. 5, pp. 1201-1216, 2018. https://doi.org/10.1039/C8BM00096D
[113] B. A. Larsen, M. A. Haag, N. J. Serkova, K. R. Shroyer, and C. R. Stoldt, “Controlled aggregation of superparamagnetic iron oxide nanoparticles for the development of molecular magnetic resonance imaging probes,” Nanotechnology, vol. 19, no. 26, p. 265102, 2008. https://doi.org/10.1088/0957-4484/19/26/265102
[114] S. Dixit et al., “Phospholipid micelle encapsulated gadolinium oxide nanoparticles for imaging and gene delivery,” RSC Adv., vol. 3, no. 8, pp. 2727-2735, 2013. https://doi.org/10.1039/c2ra22293k
[115] E. Musielak, A. Feliczak-Guzik, and I. Nowak, “Synthesis and potential applications of lipid nanoparticles in medicine,” Materials (Basel)., vol. 15, no. 2, p. 682, 2022. https://doi.org/10.3390/ma15020682
[116] H. Yuan, J. Miao, Y.-Z. Du, J. You, F.-Q. Hu, and S. Zeng, “Cellular uptake of solid lipid nanoparticles and cytotoxicity of encapsulated paclitaxel in A549 cancer cells,” Int. J. Pharm., vol. 348, no. 1-2, pp. 137-145, 2008. https://doi.org/10.1016/j.ijpharm.2007.07.012
[117] Y. Kuang et al., “Hydrophobic IR-780 dye encapsulated in cRGD-conjugated solid lipid nanoparticles for NIR imaging-guided photothermal therapy,” ACS Appl. Mater. Interfaces, vol. 9, no. 14, pp. 12217-12226, 2017. https://doi.org/10.1021/acsami.6b16705
[118] J. Sun et al., “Gadolinium-loaded solid lipid nanoparticles as a tumor-absorbable contrast agent for early diagnosis of colorectal tumors using magnetic resonance colonography,” J. Biomed. Nanotechnol., vol. 12, no. 9, pp. 1709-1723, 2016. https://doi.org/10.1166/jbn.2016.2285
[119] S. Ghiani et al., “In vivo tumor targeting and biodistribution evaluation of paramagnetic solid lipid nanoparticles for magnetic resonance imaging,” Nanomedicine Nanotechnology, Biol. Med., vol. 13, no. 2, pp. 693-700, 2017. https://doi.org/10.1016/j.nano.2016.09.012
[120] P. Cai et al., “Inherently PET/CT dual modality imaging lipid nanocapsules for early detection of orthotopic lung tumors,” ACS Appl. Bio Mater., vol. 3, no. 1, pp. 611-621, 2019. https://doi.org/10.1021/acsabm.9b00993