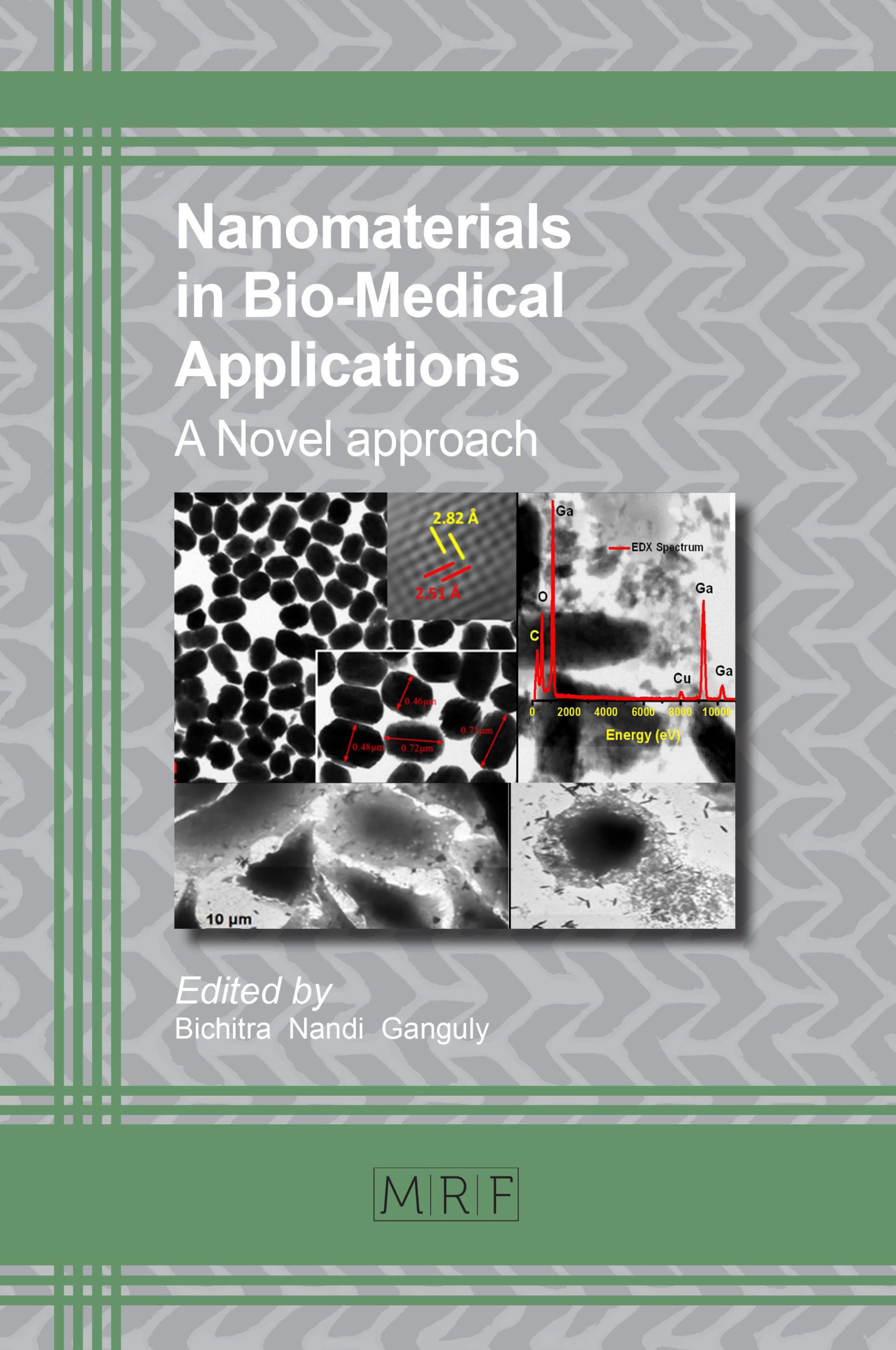
Introduction to Nano-Materials in Bio-Medical Applications: A Novel Approach
Bichitra Nandi Ganguly
Nanoparticles (NPs) have evolved as novel and valuable functional building structures, notably being considered as one of the most relevant recent achievements in materials science. With an ever growing interaction between interface-research on nanoparticles and biomedicine, materials scientists are required to encounter new and exciting challenges both in the design and engineering of the material considering its targeted application.
Keywords
Nanomaterials, Bio-Medical Applications
Published online 7/1/2018, 16 pages
DOI: http://dx.doi.org/10.21741/9781945291739-1
Part of the book on Nanomaterials in Bio-Medical Applications
References
[1] Juan J. Giner –Casares, Malou Henriksen-Lacey, Marc Coronado-Puchau and Luis M. Liz-Marzán, Inorganic nanoparticles for biomedicine: where materials scientists meet medical research, Materials Today 19 (2016) 19-28. https://doi.org/10.1016/j.mattod.2015.07.004
[2] Y.X.J. Wang, S.M. Hussain, G.P.Kretin, Supramagnetic iron oxide contrast agents: Physiochemical characteristics and applications in MR imaging , Eur. Radiol. 11 (2001) 2319-2331. https://doi.org/10.1007/s003300100908
[3] O.V.Salata, Applications of nanoparticles in biology and medicine, Journal of Nanobiotechnology 2 (2004) 3-6. https://doi.org/10.1186/1477-3155-2-3
[4] Kristof Zarschler, Louise Rocks, Nadia Licciardello, Luca Boselli, Ester Polo, P, Karina Pombo Garcia, Luisa De Cola, Holger Stephan, Kenneth A. Dawson, Kristof Zarschler, Louise Rocks, Nadia Licciardello, Luca Boselli, Ester Polo, Karina Pombo Garcia, Luisa De Cola, Holger Stephan, Kenneth A. Dawson, Ultrasmall inorganic nanoparticles: State-of-the-art and perspectives for biomedical applications, Nanomedicine: Nanotechnology, Biology, and Medicine, 12 (2016) 1663–1701. https://doi.org/10.1016/j.nano.2016.02.019
[5] W.J. Parak, D.Gerion, T. Pellegrino, D. Zanchet, C. Micheel, C.S. Williams, R. Boudreau, M.A. Le Gros, C.A. Larabell, A.P. Alivisatos, Biological applications of colloidal nanocrystals, Nanotechnology 14( 2003) R15-R27. https://doi.org/10.1088/0957-4484/14/7/201
[6] Q.A. Pankhurst, J. Connolly, S.K. Jones, J.Dobson, Applications of magnetic nanoparticles in biomedicine, J Phys D: Appl Phys., 36 (2003) R167-R181. https://doi.org/10.1088/0022-3727/36/13/201
[7] R Weissleder, G Elizondo, J Wittenburg, C.A. Rabito, H.H. Bengele, L. Josephson, Ultrasmall superparamagnetic iron oxide: char acterization of a new class of contrast agents for MR imaging. Radiology, 175 (1990) 489-493. https://doi.org/10.1148/radiology.175.2.2326474
[8] M.A. Garcia, Surface plasmons in metallic nanoparticles: fundamentals and applications, J. Phys. D: Appl. Phys., 44 (2011) 283001-2833019. https://doi.org/10.1088/0022-3727/44/28/283001
[9] M. Rubul, F.Daniel Moyano, Subinoy Rana, and Vincent M. Rotello, Surface functionalization of nanoparticles for nanomedicine, Chem Soc Rev., 41( 2012) 2539–2544. https://doi.org/10.1039/c2cs15294k
[10] A.L. Martin, L.M. Bernas, B.K. Rutt, P.J. Foster, E.R. Gillies, Enhanced cell uptake of superparamagnetic iron oxide nanoparticles functionalized with dendritic guanidines., Bioconjug Chem, 19 ( 2008) 2375–2384. https://doi.org/10.1021/bc800209u
[11] B. Kim, G Han, B.J. Toley, C.K. Kim, V.M. Rotello, N.S. Forbes, Tuning payload delivery in tumour cylindroids using gold nanoparticles. Nat Nanotechnology, 5 (2010) 465–472. https://doi.org/10.1038/nnano.2010.58
[12] K. El-Boubbou, D.C. Zhu, C. Vasileiou, B. Borhan, D. Prosperi, W. Li, X.J. Huang, Magnetic glyco-nanoparticles: a tool to detect, differentiate, and unlock the glyco-codes of cancer via magnetic resonance imaging, Am Chem Soc.,132 ( 2010) 4490– 4499. https://doi.org/10.1021/ja100455c
[13] W. John Rasmussen, Ezequiel Martinez, Panagiota Louka, and Denise G. Wingett, Zinc Oxide Nanoparticles for Selective Destruction of Tumor Cells and Potential for Drug Delivery Applications, Expert Opin Drug Deliv., 7 (2010 ) 1063–1077. https://doi.org/10.1517/17425247.2010.502560
[14] Seung Won Shin, In Hyun Song, and Soong Ho Um, Role of Physicochemical Properties in Nanoparticle Toxicity, Nanomaterials 5 ( 2015) 1351-1365. https://doi.org/10.3390/nano5031351
[15] Y. Pan, S. Neuss, A. Leifert, M. Fischler, F. Wen, U Simon, G. Schmid, W. Brandau, W Jahnen-Dechent, Size-dependent cytotoxicity of gold nanoparticles, Small, 3 ( 2007) 1941–1949. https://doi.org/10.1002/smll.200700378
[16] D. Napierska, L.C. Thomassen, V. Rabolli, D.Lison, L. Gonzalez, M.Kirsch-Volders, J.A.Martens, P.H. Hoet, Size-dependent cytotoxicity of monodisperse silica nanoparticles in human endothelial cells., Small, 5 (2009) 846–853. https://doi.org/10.1002/smll.200800461
[17] C.Carlson, S.M. Hussain, A.M. Schrand, K. L. Braydich-Stolle, K.L. Hess, R.L. Jones, J.J. Schlager, Unique cellular interaction of silver nanoparticles: Size-dependent generation of reactive oxygen species., J. Phys. Chem. B 112 (2008), 13608–13619. https://doi.org/10.1021/jp712087m
[18] M Czajka, K. Sawicki, K Sikorska, S. Popek, M.Kruszewski, L.Kapka-Skrzypczak, Toxicity of titanium dioxide nanoparticles in central nervous system. Toxicol In Vitro, 29 (2015) 1042-1052. https://doi.org/10.1016/j.tiv.2015.04.004
[19] K.Kawata ,M. Osawa, S.Okabe, In vitro toxicity of silver nanoparticles at noncytotoxic doses to HepG2 human hepatoma cells, Environmental Science and Environ Sci Technol., 43 (2009) 6046-6051. https://doi.org/10.1021/es900754q
[20] C Carlson, S.M. Hussain, A.M. Schrand, L.K. Braydich-Stolle, K.L. Hess, R.L. Jones, J.J. Schlager, Unique cellular interaction of silver nanoparticles: size-dependent generation of reactive oxygen species., J Phys Chem B. 112(2008)13608-136019. https://doi.org/10.1021/jp712087m
[21] G. Oberdörster, E. Oberdörster, J.Oberdörster, Nanotoxicology: An emerging discipline evolving from studies of ultrafine particles. Environ. Health Perspect, 113 (2005) 823–839. https://doi.org/10.1289/ehp.7339
[22] R.D. Handy, R. Owen, E. Valsami-Jones, The ecotoxicology of nanoparticles and nanomaterials: Current status, knowledge gaps, challenges, and future needs, Ecotoxicology, 17( 2008) 315–325. https://doi.org/10.1007/s10646-008-0206-0
[23] S. Hussain, K. Hess, J. Gearhart, K. Geiss, J.Schlager, In vitro toxicity of nanoparticles in BRL 3A rat liver cells. Toxicol. Vitr., 19( 2005) 975–983. https://doi.org/10.1016/j.tiv.2005.06.034
[24] J.S. Brown, K.L. Zeman, W.D. Bennett, Ultrafine particle deposition and clearance in the healthy and obstructed lung, Am. J. Respir. Crit. Care Med.,166 ( 2002), 1240–1247. https://doi.org/10.1164/rccm.200205-399OC
[25] M.P. Holsapple, W.H. Farland, T.D. Landry, N.A. Monteiro-Riviere, J.M. Carter, N.J. Walker, K.V. Thomas, Research strategies for safety evaluation of nanomaterials, part ii: Toxicological and safety evaluation of nanomaterials, current challenges and data needs, Toxicol. Sci., 88 (2005) 12–17. https://doi.org/10.1093/toxsci/kfi293
[26] A. Hoshino, K. Fujioka, T. Oku, S. Nakamura, M. Suga, Y. Yamaguchi, K. Suzuki, M. Yasuhara, K. Yamamoto, Quantum dots targeted to the assigned organelle in living cells. Microbiol. Immunol, 48( 2004) 985–994. https://doi.org/10.1111/j.1348-0421.2004.tb03621.x
[27] V. Salnikov, Y. Lukyanenko, C. Frederick, W. Lederer, V. Lukyanenko,. Probing the outer mitochondrial membrane in cardiac mitochondria with nanoparticles. Biophys., J. 2007(92) 1058–1071. https://doi.org/10.1529/biophysj.106.094318
[28] K. Donaldson, V. Stone, Current hypotheses on the mechanisms of toxicity of ultrafine particles, Ann. Ist. Super. Sanita , 39 (2002) 405–410.
[29] R.F. Wilson, Nanotechnology: The challenge of regulating known unknowns. J. Law Med. Ethics, 34 (2006) 704–713. https://doi.org/10.1111/j.1748-720X.2006.00090.x
[30] L.Y. Chou, K. Zagorovsky, W.C. Chan, DNA assembly of nanoparticle superstructures for controlled biological delivery and elimination, Nat Nanotechnol, 9 (2014) 148-155. https://doi.org/10.1038/nnano.2013.309
[31] S.Yang, S. Sun, C. Zhou, G. Hao, J. Liu, S. Ramezani, et al., Renal clearance and degradation of glutathione-coated copper nanoparticles., Bioconjug Chem., 26(2015) 511-519. https://doi.org/10.1021/acs.bioconjchem.5b00003
[32] J.M. Tam, J.O. Tam, A. Murthy, D.R. Ingram, L.L. Ma, K. Travis, et al., Controlled assembly of biodegradable plasmonic nanoclusters for near infrared imaging and therapeutic applications., ACS Nano , 4 (2010) 2178-2184. https://doi.org/10.1021/nn9015746
[33] Bichitra Nandi Ganguly, Buddhadeb Maity, Tapan Kumar Maity, Joydeb Manna, Modhusudan Roy, Manabendra Mukherjee, et al., L-Cysteine-Conjugated Ruthenium Hydrous Oxide Nanomaterials with Anticancer Active Application, Langmuir, 4 (2018) 1447-1456. https://doi.org/10.1021/acs.langmuir.7b01408
[34] Bichitra Nandi Ganguly, Vivek Verma, Debanuj Chatterjee, Biswarup Satpati, Sushanta Debnath and Partha Saha, Study of Gallium Oxide Nanoparticles Conjugated with -cyclodextrin -An Application to Combat Cancer, ACS Materials and Interfaces 8 (2016) ,17127- 17137. https://doi.org/10.1021/acsami.6b04807
[35] Sreetama Dutta and Bichitra N Ganguly, Characterization of ZnO nano particles grown in presence of Folic Acid template, J. Nanobiotechnology 10 (2012), 29-38. https://doi.org/10.1186/1477-3155-10-29
[36] S. Huo, H. Ma, K. Huang, Superior penetration and retention behavior of 50 nm gold nanoparticles in tumors, Cancer Res 73 (2013), 319-330. https://doi.org/10.1158/0008-5472.CAN-12-2071
[37] J.M. Montenegro, V Grazu, A Sukhanova, S .Agarwal, JM de la Fuente, I. Nabiev, A. Greiner, W.J. Parak., Controlled antibody/(bio-) conjugation of inorganic nanoparticles for targeted delivery, Adv Drug Deliv Rev., 65 (2013), 677- 688. https://doi.org/10.1016/j.addr.2012.12.003
[38] Diana Dehaini, H. Ronnie Fang, Liangfang Zhang, Biomimetic strategies for targeted nanoparticle delivery, Bioengineering and translational medicine, 1 (2016) 30–46.
[39] M. Jansch, P. .Stumpf, C. Graf, E. Ruhl, R.H. Muller, Adsorption kinetics of plasma proteins on ultrasmall superparamagnetic iron oxide (USPIO) nanoparticles., Int J Pharm , 428 (2012) 125-133. https://doi.org/10.1016/j.ijpharm.2012.01.060
[40] P. Maffre, S. Brandholt, K. Nienhaus, L. Shang, W.J. Parak, G.U. Nienhaus, Effects of surface functionalization on the adsorption of human serum albumin onto nanoparticles – a fluorescence correlation spectroscopy study, Beilstein J Nanotechnol., 5 ( 2014) 2036-2047. https://doi.org/10.3762/bjnano.5.212
[41] A. Salvati, A.S. Pitek, M.P. Monopoli, K. Prapainop, F.B. Bombelli, D.R. Hristov, et al. Transferrin-functionalized nanoparticles lose their targeting capabilities when a biomolecule corona adsorbs on the surface, Nat Nanotechnol, 8 (2013) 137-143. https://doi.org/10.1038/nnano.2012.237
[42] A. Lesniak, F. Fenaroli, M.P. Monopoli, C. Åberg, K.A. Dawson, A. Salvati, Effects of the presence or absence of a protein corona on silica nanoparticle uptake and impact on cells, ACS Nano, 6 (2012) 5845-5857. https://doi.org/10.1021/nn300223w
[43] M.P. Monopoli, CÅberg, A. Salvati, K.A. Dawson, Biomolecular coronas provide the biological identity of nanosized materials, Nat Nanotechnol, 7(2012) 79-86. https://doi.org/10.1038/nnano.2012.207
[44] S.C. Baetke, T .Lammers, F. Kiessling, Applications of nanoparticles for diagnosis and therapy of cancer, Br J Radiol, (2015):20150207. https://doi.org/10.1259/bjr.20150207
[45] J.V. Frangioni, New technologies for human cancer imaging, J Clin Oncol, 26 (2008) 4012- 4021. https://doi.org/10.1200/JCO.2007.14.3065
[46] X. Tan, R Jin, Ultrasmall metal nanoclusters for bio-related applications. Wiley Interdiscip Rev Nanomed Nanobiotechnol., 5 (2013) 569-581. https://doi.org/10.1002/wnan.1237
[47] O. Khani, H.R. Rajabi, M.H.Yousefi, A.A. Khosravi, M.Jannesari, M Shamsipur, Synthesis and characterizations of ultra-small ZnS and Zn(1-x)Fe(x)S quantum dots in aqueous media and spectroscopic study of their interactions with bovine serum albumin, Spectrochim Acta A Mol Biomol Spectrosc .,79 (2011) 361-369. https://doi.org/10.1016/j.saa.2011.03.025
[48] T. Xuan, S. Wang, X. Wang, J. Liu, J. Chen, H. Li, et al., Single-step noninjection synthesis of highly luminescent water soluble Cu+ doped CdS quantum dots: Application as bio-imaging agents, Chem Commun (Camb), 49 ( 2013) 9045-9047. https://doi.org/10.1039/c3cc44601h
[49] L.N. Chen, J. Wang, W.T. Li, H.Y. Han, Aqueous one-pot synthesis of bright and ultrasmall CdTe/CdS near-infrared-emitting quantum dots and their application for tumor targeting in vivo, Chem Commun (Camb), 48 (2012) 4971-4973. https://doi.org/10.1039/c2cc31259j
[50] Y. Li, Z. Li, X. Wang, F. Liu, Y. Cheng, B. Zhang, et al., In vivo cancer targeting and imaging-guided surgery with near infrared-emitting quantum dot bioconjugates, Theranostics, 2 (2012) 769-776. https://doi.org/10.7150/thno.4690
[51] K. Ma, H. Sai, U. Wiesner, Ultrasmall sub-10 nm near-infrared fluorescent mesoporous silica nanoparticles, J Am Chem Soc, 134 (2012), 13180-131803. https://doi.org/10.1021/ja3049783
[52] C. .Zhou, G. Hao, P. Thomas, J. Liu, M. Yu, S. Sun, et al., Near-infrared emitting radioactive gold nanoparticles with molecular pharmacokinetics, Angew Chem Int Ed Engl, 51 (2012) 10118- 10122.
[53] A. Mignot, C. Truillet, F. Lux, L. Sancey, C. Louis, F. Denat, et al., A top down synthesis route to ultrasmall multifunctional Gd-based silica nanoparticles for theranostic applications, Chemistry, 19 (2013) 6122-6136. https://doi.org/10.1002/chem.201203003
[54] M.S. Bradbury, E. Phillips, P.H. Montero, S.M. Cheal, H. Stambuk, J.C. Durack, et al., Clinically-translated silica nanoparticles as dual-modality cancer-targeted probes for image-guided surgery and interventions, Integr Biol (Camb), 5 (2013) 54-86. https://doi.org/10.1039/C2IB20174G
[55] Kotb Shady, Alexandre Detappe, Florence Appaix, L. Emmanuel. Barbier, Vu-Long Tran, Marie Plissonneau, Hélène Gehan, Florence Lefranc, Claire Rodriguez-Lafrasse, Camille Verry, Ross Berbeco, Olivier Tillement, and Lucie Sancey, Gadolinium-Based Nanoparticles and Radiation Therapy for Multiple Brain Melanoma Metastases: Proof of Concept before Phase I Trial, Theranostics, 6 (2016) 418–427. https://doi.org/10.7150/thno.14018
[56] Y. Li, Z. Li, X. Wang, F. Liu, Y. Cheng, B. Zhang, et al., In vivo cancer targeting and imaging-guided surgery with near infrared-emitting quantum dot bioconjugates. Theranostics, 2 (2012) 769-776. https://doi.org/10.7150/thno.4690
[57] Y. Zhao, D. Sultan, L. Detering, H. Luehmann, Y. Liu, Facile synthesis, pharmacokinetic and systemic clearance evaluation, and positron emission tomography cancer imaging of 64Cu-Au alloy nanoclusters., Nanoscale, 6 (2014) 13501-13509. https://doi.org/10.1039/C4NR04569F
[58] F. Gao, P Cai, W.Yang, J. Xue, L. Gao, R. Liu, et al., Ultrasmall [64Cu]Cu nanoclusters for targeting orthotopic lung tumors using accurate positron emission tomography imaging., ACS Nano, 9 (2015) 4976-4986. https://doi.org/10.1021/nn507130k
[59] M. Zhou, J. Li, S. Liang, A.K. Sood, D. Liang, C. Li,. CuS nanodots with ultrahigh efficient renal clearance for positron emission tomography imaging and image-guided photothermal therapy, ACS Nano, 9 (2015) 7085-96. https://doi.org/10.1021/acsnano.5b02635
[60] R. Chakravarty, S. Goel, A. Dash, W. Cai, Radiolabeled inorganic nanoparticles for positron emission tomography imaging of cancer: an overview, Q J Nucl Med Mol Imaging, 61 (2017) )181-204.
[61] B.N. Ganguly, N.N. Mondal, M. Nandy, F. Roesch, Some physical aspects of positron annihilation tomography: A critical review, Journal of Radioanalytical and Nuclear Chemistry, 279 (2009) 685–698. https://doi.org/10.1007/s10967-007-7256-2
[62] C. Pẻrez-Campana, Vanessa Gómez-Vallejo, Maria Puigivila, Abraham Martín, Teresa Calv, Carlos Pérez-Campañao-Fernández, Sergio E. Moya, Ronald F. Ziolo, Torsten Reese, and Jordi Llop, Biodistribution of Different Sized Nanoparticles Assessed by Positron Emission Tomography: A General Strategy for Direct Activation of Metal Oxide Particles, ACS Nano, 7(2013) 3498-350. https://doi.org/10.1021/nn400450p