Wound Treatment Using Nanomaterials
J.M. Rajwade, K. Kawle, S. Kulkarni, M. Kowshik
Skin wounds are categorized as ‘acute’ or ‘chronic’ based on the healing process. Wound care is of utmost importance as the break in the skin barrier exposes the internal milieu to various commensal and pathogenic microbes. The usage of nanomaterials is a recent approach to facilitate wound healing by processes that operate singly or in tandem. Metal based nanomaterials show antibacterial, antifungal, and anti-inflammatory activities; and organic-inorganic, organic-organic nanocomposites as ‘smart’, ‘advanced’ materials would play a crucial role in wound care. Use of nanomaterials in wound care would revolutionarize treatment, thus lowering the economic burden.
Keywords
Chronic Wounds, Nanoparticles, Wound Healing, Wound Dressings
Published online , 29 pages
Citation: J.M. Rajwade, K. Kawle, S. Kulkarni, M. Kowshik, Wound Treatment Using Nanomaterials, Materials Research Proceedings, Vol. 145, pp 207-235, 2023
DOI: https://doi.org/10.21741/9781644902370-8
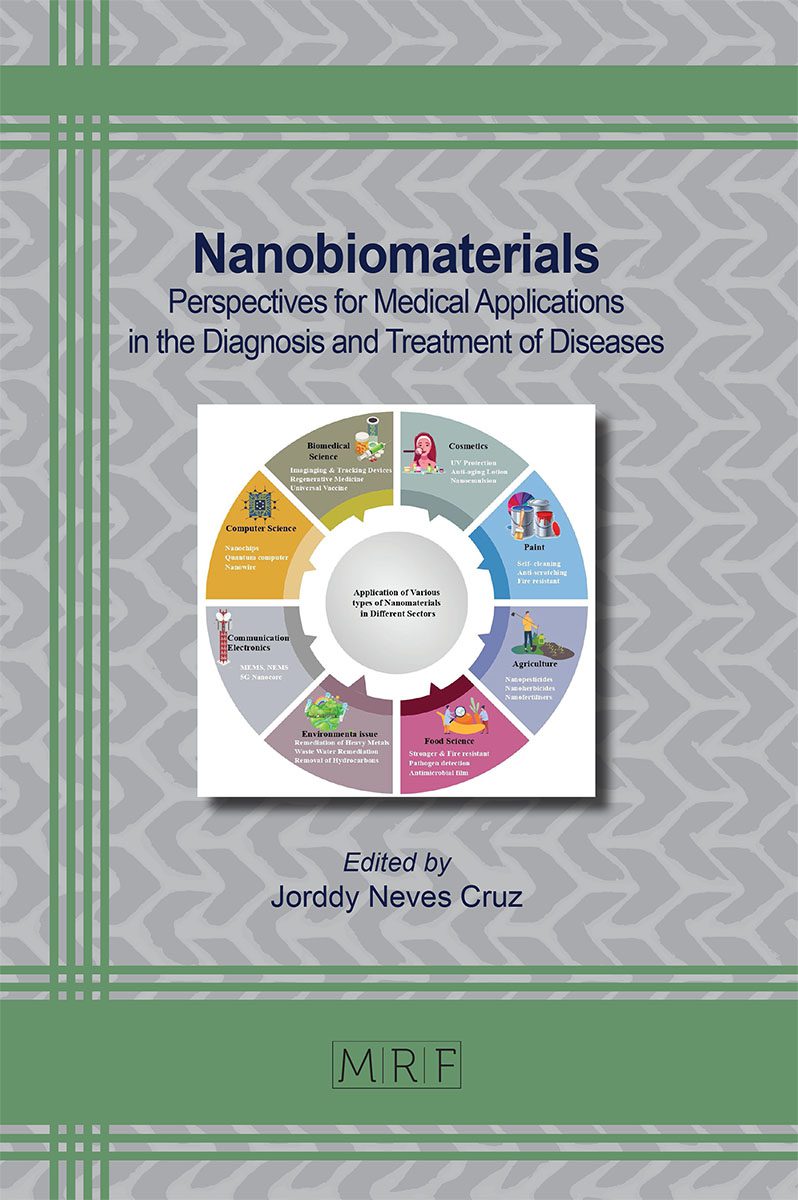
Part of the book on Nanobiomaterials
References
[1] S. Vyavahare, N. Padole, J. Avari, a Review: Silver Nanoparticles in Wound Healing, Eur. J. Pharm. Med. Res. Www.Ejpmr.Com │. 8 (2015). www.ejpmr.com
[2] E. Rezvani Ghomi, S. Khalili, S. Nouri Khorasani, R. Esmaeely Neisiany, S. Ramakrishna, Wound dressings: Current advances and future directions, J. Appl. Polym. Sci. 136 (2019) 1–12. https://doi.org/10.1002/app.47738
[3] S.N.A. Bakil, H. Kamal, H.Z. Abdullah, M.I. Idris, Sodium alginate-zinc oxide nanocomposite film for antibacterial wound healing applications, Biointerface Res. Appl. Chem. 10 (2020) 6245–6252. https://doi.org/10.33263/BRIAC105.62456252
[4] M. Wang, X. Lai, L. Shao, L. Li, Evaluation of immunoresponses and cytotoxicity from skin exposure to metallic nanoparticles, Int. J. Nanomedicine. 13 (2018) 4445–4459. https://doi.org/10.2147/IJN.S170745
[5] R. Singh, K. Shitiz, A. Singh, Chitin and chitosan: biopolymers for wound management, Int. Wound J. 14 (2017) 1276–1289. https://doi.org/10.1111/iwj.12797
[6] K. Vig, A. Chaudhari, S. Tripathi, S. Dixit, R. Sahu, S. Pillai, V.A. Dennis, S.R. Singh, Advances in skin regeneration using tissue engineering, Int. J. Mol. Sci. 18 (2017) 789. https://doi.org/10.3390/ijms18040789
[7] L.A. Schneider, A. Korber, S. Grabbe, J. Dissemond, Influence of pH on wound-healing: A new perspective for wound-therapy?, Arch. Dermatol. Res. 298 (2007) 413–420. https://doi.org/10.1007/s00403-006-0713-x
[8] S. Dhivya, V.V. Padma, E. Santhini, Wound dressings – A review, Biomed. 5 (2015) 24–28. https://doi.org/10.7603/s40681-015-0022-9
[9] A.R.J.A. de M. Lima, A.S. Siqueira, M.L.S. Möller, R.C. de Souza, J.N. Cruz, A.R.J.A. de M. Lima, R.C. da Silva, D.C.F. Aguiar, J.L. da S.G.V. Junior, E.C. Gonçalves, In silico improvement of the cyanobacterial lectin microvirin and mannose interaction, J. Biomol. Struct. Dyn. (2020). https://doi.org/10.1080/07391102.2020.1821782
[10] R. Fernández-Torres, M. Ruiz-Muñoz, A.J. Pérez-Panero, J.C. García-Romero, M. Gónzalez-Sánchez, Clinician assessment tools for patients with diabetic foot disease: A systematic review, J. Clin. Med. 9 (2020). https://doi.org/10.3390/jcm9051487
[11] J.B. Acosta, D. Garcia Del Barco, D. Cibrian Vera, W. Savigne, P. Lopez-Saura, G. Guillen Nieto, G.S. Schultz, The pro-inflammatory environment in recalcitrant diabetic foot wounds, Int. Wound J. 5 (2008) 530–539. https://doi.org/10.1111/j.1742-481X.2008.00457.x
[12] R. Blakytny, E.B. Jude, Altered molecular mechanisms of diabetic foot ulcers, Int. J. Low. Extrem. Wounds. 8 (2009) 95–104. https://doi.org/10.1177/1534734609337151
[13] M.S. Bader, Diabetic foot infection, Am. Fam. Physician. 78 (2008)
[14] S.C. Mishra, K.C. Chhatbar, A. Kashikar, A. Mehndiratta, Diabetic foot, BMJ. 359 (2017) j5064. https://doi.org/10.1136/bmj.j5064
[15] R. Webb, From decubitus ulcers to pressure injury: What is in a name?, J. Wound Care. 26 (2017) 3. https://doi.org/10.12968/jowc.2017.26.1.3
[16] B. Tirgari, L. Mirshekari, M.A. Forouzi, Pressure Injury Prevention: Knowledge and Attitudes of Iranian Intensive Care Nurses, Adv. Ski. Wound Care. 31 (2018) 1–8. https://doi.org/10.1097/01.ASW.0000530848.50085.ef
[17] C.D. Weller, E.R. Gershenzon, S.M. Evans, V. Team, J.J. McNeil, Pressure injury identification, measurement, coding, and reporting: Key challenges and opportunities, Int. Wound J. 15 (2018) 417–423. https://doi.org/10.1111/iwj.12879
[18] S. Natarajan, D. Williamson, A.J. Stiltz, K.G. Harding, Advances in wound care and healing technology, Am. J. Clin. Dermatol. 1 (2000) 269–275. https://doi.org/10.2165/00128071-200001050-00002
[19] S. Palfreyman, E.A. Nelson, J.A. Michaels, Dressings for venous leg ulcers: Systematic review and meta-analysis, Br. Med. J. 335 (2007) 244–248. https://doi.org/10.1136/bmj.39248.634977.AE
[20] S. Chapman, Venous leg ulcers: An evidence review, Br. J. Community Nurs. 22 (2017) S6–S9. https://doi.org/10.12968/bjcn.2017.22.Sup9.S6
[21] S.A.M. Elgayar, O.A. Hussein, H.A. Mubarak, A.M. Ismaiel, A.M.S. Gomaa, Testing efficacy of the nicotine protection of the substantia nigra pars compacta in a rat Parkinson disease model. Ultrastructure study, Ultrastruct. Pathol. 46 (2022) 37–53. https://doi.org/10.1080/01913123.2021.2015499
[22] J. Boateng, M. Verghese, L.T. Walker, S. Ogutu, Effect of processing on antioxidant contents in selected dry beans (Phaseolus spp. L.), Lwt. 41 (2008) 1541–1547. https://doi.org/10.1016/j.lwt.2007.11.025
[23] F.S. Lozano Sánchez, J. Marinel lo Roura, E. Carrasco Carrasco, J.R. González-Porras, J.R. Escudero Rodríguez, I. Sánchez Nevarez, S. Díaz Sánchez, Venous leg ulcer in the context of chronic venous disease, Phlebology. 29 (2014) 220–226. https://doi.org/10.1177/0268355513480489
[24] J.D. Raffetto, Dermal pathology, cellular biology, and inflammation in chronic venous disease, Thromb. Res. 123 (2009) S66–S71. https://doi.org/10.1016/S0049-3848(09)70147-1
[25] K. Khezri, M.R. Farahpour, S. Mounesi Rad, Efficacy of Mentha pulegium essential oil encapsulated into nanostructured lipid carriers as an in vitro antibacterial and infected wound healing agent, Colloids Surfaces A Physicochem. Eng. Asp. 589 (2020) 124414. https://doi.org/10.1016/j.colsurfa.2020.124414
[26] D. Stavrou, O. Weissman, A. Tessone, I. Zilinsky, S. Holloway, J. Boyd, J. Haik, Health Related Quality of Life in burn patients – A review of the literature, Burns. 40 (2014) 788–796. https://doi.org/10.1016/j.burns.2013.11.014
[27] S. Hettiaratchy, P. Dziewulski, Pathophysiology and types of burns, Bmj. 328 (2004) 1427. https://doi.org/10.1136/bmj.328.7453.1427
[28] H.J. Klasen, A historical review of the use of silver in the treatment of burns. II. Renewed interest for silver, Burns. 26 (2000) 131–138. https://doi.org/10.1016/S0305-4179(99)00116-3
[29] C. Shi, C. Wang, H. Liu, Q. Li, R. Li, Y. Zhang, Y. Liu, Y. Shao, J. Wang, Selection of Appropriate Wound Dressing for Various Wounds, Front. Bioeng. Biotechnol. 8 (2020) 1–17. https://doi.org/10.3389/fbioe.2020.00182
[30] J. Wang, J. Tavakoli, Y. Tang, Bacterial cellulose production, properties and applications with different culture methods – A review, Carbohydr. Polym. 219 (2019) 63–76. https://doi.org/10.1016/j.carbpol.2019.05.008
[31] S. Saghazadeh, C. Rinoldi, M. Schot, S.S. Kashaf, F. Sharifi, E. Jalilian, K. Nuutila, G. Giatsidis, P. Mostafalu, H. Derakhshandeh, K. Yue, W. Swieszkowski, A. Memic, A. Tamayol, A. Khademhosseini, Drug delivery systems and materials for wound healing applications, Adv. Drug Deliv. Rev. 127 (2018) 138–166. https://doi.org/10.1016/j.addr.2018.04.008
[32] P. Victor, D. Sarada, K.M. Ramkumar, Pharmacological activation of Nrf2 promotes wound healing, Eur. J. Pharmacol. 886 (2020) 173395. https://doi.org/10.1016/j.ejphar.2020.173395
[33] M.T. Matter, S. Probst, S. Läuchli, I.K. Herrmann, Uniting drug and delivery: Metal oxide hybrid nanotherapeutics for skin wound care, Pharmaceutics. 12 (2020) 1–17. https://doi.org/10.3390/pharmaceutics12080780
[34] A. Kushwaha, L. Goswami, B.S. Kim, Nanomaterial-Based Therapy for Wound Healing, Nanomaterials. 12 (2022). https://doi.org/10.3390/nano12040618
[35] F. Thiruvoth, D. Mohapatra, D. Sivakumar, R. Chittoria, V. Nandhagopal, Current concepts in the physiology of adult wound healing, Plast. Aesthetic Res. 2 (2015) 250. https://doi.org/10.4103/2347-9264.158851
[36] L.I.F. Moura, A.M.A. Dias, E. Carvalho, H.C. De Sousa, Recent advances on the development of wound dressings for diabetic foot ulcer treatment – A review, Acta Biomater. 9 (2013) 7093–7114. https://doi.org/10.1016/j.actbio.2013.03.033
[37] H.S. Kim, X. Sun, J.H. Lee, H.W. Kim, X. Fu, K.W. Leong, Advanced drug delivery systems and artificial skin grafts for skin wound healing, Adv. Drug Deliv. Rev. 146 (2019) 209–239. https://doi.org/10.1016/j.addr.2018.12.014
[38] F.S. Alves, J. de A. Rodrigues Do Rego, M.L. Da Costa, L.F. Lobato Da Silva, R.A. Da Costa, J.N. Cruz, D.D.S.B. Brasil, Spectroscopic methods and in silico analyses using density functional theory to characterize and identify piperine alkaloid crystals isolated from pepper (Piper Nigrum L.), J. Biomol. Struct. Dyn. 38 (2020) 2792–2799. https://doi.org/10.1080/07391102.2019.1639547
[39] M. Fronza, G.F. Caetano, M.N. Leite, C.S. Bitencourt, F.W.G. Paula-Silva, T.A.M. Andrade, M.A.C. Frade, I. Merfort, L.H. Faccioli, Hyaluronidase modulates inflammatory response and accelerates the cutaneous wound healing, PLoS One. 9 (2014) 1–12. https://doi.org/10.1371/journal.pone.0112297
[40] N.K. Rajendran, S.S.D. Kumar, N.N. Houreld, H. Abrahamse, A review on nanoparticle based treatment for wound healing, J. Drug Deliv. Sci. Technol. 44 (2018) 421–430. https://doi.org/10.1016/j.jddst.2018.01.009
[41] J. Li, J. Chen, R. Kirsner, Pathophysiology of acute wound healing, Clin. Dermatol. 25 (2007) 9–18. https://doi.org/10.1016/j.clindermatol.2006.09.007
[42] G.L. Brown, L.J. Curtsinger, M. White, R.O. Mitchell, J. Pietsch, R. Nordquist, A. Von Fraunhofer, G.S. Schultz, Acceleration of tensile strength of incisions treated with EGF and TGF-β, Ann. Surg. 208 (1988) 788–794. https://doi.org/10.1097/00000658-198812000-00019
[43] P.I. Morgado, A. Aguiar-Ricardo, I.J. Correia, Asymmetric membranes as ideal wound dressings: An overview on production methods, structure, properties and performance relationship, J. Memb. Sci. 490 (2015) 139–151. https://doi.org/10.1016/j.memsci.2015.04.064
[44] M. Xue, C.J. Jackson, Extracellular Matrix Reorganization During Wound Healing and Its Impact on Abnormal Scarring, Adv. Wound Care. 4 (2015) 119–136. https://doi.org/10.1089/wound.2013.0485
[45] S. Nam, D. Mooney, Polymeric Tissue Adhesives, Chem. Rev. 121 (2021) 11336–11384. https://doi.org/10.1021/acs.chemrev.0c00798
[46] G. Yang, Z. Zhang, K. Liu, X. Ji, P. Fatehi, J. Chen, A cellulose nanofibril-reinforced hydrogel with robust mechanical, self-healing, pH-responsive and antibacterial characteristics for wound dressing applications, J. Nanobiotechnology. 20 (2022) 1–16. https://doi.org/10.1186/s12951-022-01523-5
[47] Q. Zeng, X. Qi, G. Shi, M. Zhang, H. Haick, Wound Dressing: From Nanomaterials to Diagnostic Dressings and Healing Evaluations, ACS Nano. 16 (2022) 1708–1733. https://doi.org/10.1021/acsnano.1c08411
[48] G. Dabiri, E. Damstetter, T. Phillips, Choosing a Wound Dressing Based on Common Wound Characteristics, Adv. Wound Care. 5 (2016) 32–41. https://doi.org/10.1089/wound.2014.0586
[49] D. Simões, S.P. Miguel, M.P. Ribeiro, P. Coutinho, A.G. Mendonça, I.J. Correia, Recent advances on antimicrobial wound dressing: A review, Eur. J. Pharm. Biopharm. 127 (2018) 130–141. https://doi.org/10.1016/j.ejpb.2018.02.022
[50] N. Naderi, D. Karponis, A. Mosahebi, A.M. Seifalian, Nanoparticles in wound healing; from hope to promise, from promise to routine, Front. Biosci. – Landmark. 23 (2018) 1038–1059. https://doi.org/10.2741/4632
[51] K. Kalantari, E. Mostafavi, A.M. Afifi, Z. Izadiyan, H. Jahangirian, R. Rafiee-Moghaddam, T.J. Webster, Wound dressings functionalized with silver nanoparticles: Promises and pitfalls, Nanoscale. 12 (2020) 2268–2291. https://doi.org/10.1039/c9nr08234d
[52] X.F. Zhang, W. Shen, S. Gurunathan, Silver nanoparticle-mediated cellular responses in various cell lines: An in vitro model, Int. J. Mol. Sci. 17 (2016) 1–26. https://doi.org/10.3390/ijms17101603
[53] J. Jain, S. Arora, J.M. Rajwade, P. Omray, S. Khandelwal, K.M. Paknikar, Silver nanoparticles in therapeutics: Development of an antimicrobial gel formulation for topical use, Mol. Pharm. 6 (2009) 1388–1401. https://doi.org/10.1021/mp900056g
[54] J. Sheikh, I. Bramhecha, Multi-functionalization of linen fabric using a combination of chitosan, silver nanoparticles and Tamarindus Indica L. seed coat extract, Cellulose. 26 (2019) 8895–8905. https://doi.org/10.1007/s10570-019-02684-7
[55] S. Li, A. Chen, Y. Chen, Y. Yang, Q. Zhang, S. Luo, M. Ye, Y. Zhou, Y. An, W. Huang, T. Xuan, Y. Pan, X. Xuan, H. He, J. Wu, Lotus leaf inspired antiadhesive and antibacterial gauze for enhanced infected dermal wound regeneration, Chem. Eng. J. 402 (2020) 126202. https://doi.org/10.1016/j.cej.2020.126202
[56] K. Brindhadevi, B.H. Elesawy, A. Elfasakhany, I.A. Badruddin, S. Kamangar, Wound dressings coated with silver nanoparticles and essential oil of Labdanum, Appl. Nanosci. (2021). https://doi.org/10.1007/s13204-021-02040-x
[57] C. Rigo, L. Ferroni, I. Tocco, M. Roman, I. Munivrana, C. Gardin, W.R.L. Cairns, V. Vindigni, B. Azzena, C. Barbante, B. Zavan, Active silver nanoparticles for wound healing, Int. J. Mol. Sci. 14 (2013) 4817–4840. https://doi.org/10.3390/ijms14034817
[58] H. Choudhury, M. Pandey, Y.Q. Lim, C.Y. Low, C.T. Lee, T.C.L. Marilyn, H.S. Loh, Y.P. Lim, C.F. Lee, S.K. Bhattamishra, P. Kesharwani, B. Gorain, Silver nanoparticles: Advanced and promising technology in diabetic wound therapy, Mater. Sci. Eng. C. 112 (2020) 110925. https://doi.org/10.1016/j.msec.2020.110925
[59] M. Konop, J. Czuwara, E. Kłodzińska, A.K. Laskowska, D. Sulejczak, T. Damps, U. Zielenkiewicz, I. Brzozowska, A. Sureda, T. Kowalkowski, R.A. Schwartz, L. Rudnicka, Evaluation of keratin biomaterial containing silver nanoparticles as a potential wound dressing in full-thickness skin wound model in diabetic mice, J. Tissue Eng. Regen. Med. 14 (2020) 334–346. https://doi.org/10.1002/term.2998
[60] A. Naskar, K.S. Kim, Recent advances in nanomaterial-based wound-healing therapeutics, Pharmaceutics. 12 (2020). https://doi.org/10.3390/pharmaceutics12060499
[61] J. Xiang, R. Zhu, S. Lang, H. Yan, G. Liu, B. Peng, Mussel-inspired immobilization of zwitterionic silver nanoparticles toward antibacterial cotton gauze for promoting wound healing, Chem. Eng. J. 409 (2021) 128291. https://doi.org/10.1016/j.cej.2020.128291
[62] M. Khatami, R.S. Varma, N. Zafarnia, H. Yaghoobi, M. Sarani, V.G. Kumar, Applications of green synthesized Ag, ZnO and Ag/ZnO nanoparticles for making clinical antimicrobial wound-healing bandages, Sustain. Chem. Pharm. 10 (2018) 9–15. https://doi.org/10.1016/j.scp.2018.08.001
[63] A.Y.H. Nor Azlan, H. Katas, M.F. Mh Busra, N.A.M. Salleh, A. Smandri, Metal nanoparticles and biomaterials: The multipronged approach for potential diabetic wound therapy, Nanotechnol. Rev. 10 (2021) 653–670. https://doi.org/10.1515/ntrev-2021-0046
[64] J. Tian, K.K.Y. Wong, C.M. Ho, C.N. Lok, W.Y. Yu, C.M. Che, J.F. Chiu, P.K.H. Tam, Topical delivery of silver nanoparticles promotes wound healing, ChemMedChem. 2 (2007) 129–136. https://doi.org/10.1002/cmdc.200600171
[65] M.M. Mihai, M.B. Dima, B. Dima, A.M. Holban, Nanomaterials for wound healing and infection control, Materials (Basel). 12 (2019) 2176. https://doi.org/10.3390/ma12132176
[66] A. Damle, R. Sundaresan, J.M. Rajwade, P. Srivastava, A. Naik, A concise review on implications of silver nanoparticles in bone tissue engineering, Biomater. Adv. 141 (2022) 213099. https://doi.org/10.1016/j.bioadv.2022.213099
[67] H. Jia, X. Zeng, S. Fan, R. Cai, Z. Wang, Y. Yuan, T. Yue, Silver nanoparticles anchored magnetic self-assembled carboxymethyl cellulose-ε-polylysine hybrids with synergetic antibacterial activity for wound infection therapy, Int. J. Biol. Macromol. 210 (2022) 703–715. https://doi.org/10.1016/j.ijbiomac.2022.04.225
[68] J.G. Leu, S.A. Chen, H.M. Chen, W.M. Wu, C.F. Hung, Y. Der Yao, C.S. Tu, Y.J. Liang, The effects of gold nanoparticles in wound healing with antioxidant epigallocatechin gallate and α-lipoic acid, Nanomedicine Nanotechnology, Biol. Med. 8 (2012) 767–775. https://doi.org/10.1016/j.nano.2011.08.013
[69] P.S. Lau, N. Bidin, S. Islam, W.N.B.W.M. Shukri, N. Zakaria, N. Musa, G. Krishnan, Influence of gold nanoparticles on wound healing treatment in rat model: Photobiomodulation therapy, Lasers Surg. Med. 49 (2017) 380–386. https://doi.org/10.1002/lsm.22614
[70] M.M. Abousamra, A. Mona M, Citation: Abousamra MM. Nanoparticles as Safe and Effective Drug Delivery Systems for Wound Healing, Austin J Nanomed Nanotechnol. 7 (2019) 1–10. www.austinpublishinggroup.com
[71] O. Akturk, K. Kismet, A.C. Yasti, S. Kuru, M.E. Duymus, F. Kaya, M. Caydere, S. Hucumenoglu, D. Keskin, Collagen/gold nanoparticle nanocomposites: A potential skin wound healing biomaterial, J. Biomater. Appl. 31 (2016) 283–301. https://doi.org/10.1177/0885328216644536
[72] S.P.H. Martínez, T.I.R. González, M.A.F. Molina, J.J. Bollain Y Goytia, J.J.M. Sanmiguel, D.G.Z. Triviño, C.R. Padilla, A novel gold calreticulin nanocomposite based on chitosan for wound healing in a diabetic mice model, Nanomaterials. 9 (2019) 75. https://doi.org/10.3390/nano9010075
[73] J. Salvo, C. Sandoval, Role of copper nanoparticles in wound healing for chronic wounds: Literature review, Burn. Trauma. 10 (2022). https://doi.org/10.1093/burnst/tkab047
[74] S.K. Nethi, S. Das, C.R. Patra, S. Mukherjee, Recent advances in inorganic nanomaterials for wound-healing applications, Biomater. Sci. 7 (2019) 2652–2674. https://doi.org/10.1039/c9bm00423h
[75] B. Tao, C. Lin, Y. Deng, Z. Yuan, X. Shen, M. Chen, Y. He, Z. Peng, Y. Hu, K. Cai, Copper-nanoparticle-embedded hydrogel for killing bacteria and promoting wound healing with photothermal therapy, J. Mater. Chem. B. 7 (2019) 2534–2548. https://doi.org/10.1039/C8TB03272F
[76] S. Jiang, B.C. Ma, W. Huang, A. Kaltbeitzel, G. Kizisavas, D. Crespy, K.A.I. Zhang, K. Landfester, Visible light active nanofibrous membrane for antibacterial wound dressing, Nanoscale Horizons. 3 (2018) 439–446. https://doi.org/10.1039/c8nh00021b
[77] R. Jose Varghese, S. Parani, V.R. Remya, R. Maluleke, S. Thomas, O.S. Oluwafemi, Sodium alginate passivated CuInS2/ZnS QDs encapsulated in the mesoporous channels of amine modified SBA 15 with excellent photostability and biocompatibility, Int. J. Biol. Macromol. 161 (2020) 1470–1474. https://doi.org/10.1016/j.ijbiomac.2020.07.240
[78] E.M. Hetrick, J.H. Shin, H.S. Paul, M.H. Schoenfisch, Anti-biofilm efficacy of nitric oxide-releasing silica nanoparticles, Biomaterials. 30 (2009) 2782–2789. https://doi.org/10.1016/j.biomaterials.2009.01.052
[79] F. Öri, R. Dietrich, C. Ganz, M. Dau, D. Wolter, A. Kasten, T. Gerber, B. Frerich, Silicon-dioxide−polyvinylpyrrolidone as a wound dressing for skin defects in a murine model, J. Cranio-Maxillofacial Surg. 45 (2017) 99–107. https://doi.org/10.1016/j.jcms.2016.10.002
[80] R. Ahmed, M. Tariq, I. Ali, R. Asghar, P. Noorunnisa Khanam, R. Augustine, A. Hasan, Novel electrospun chitosan/polyvinyl alcohol/zinc oxide nanofibrous mats with antibacterial and antioxidant properties for diabetic wound healing, Int. J. Biol. Macromol. 120 (2018) 385–393. https://doi.org/10.1016/j.ijbiomac.2018.08.057
[81] R. Pati, R.K. Mehta, S. Mohanty, A. Padhi, M. Sengupta, B. Vaseeharan, C. Goswami, A. Sonawane, Topical application of zinc oxide nanoparticles reduces bacterial skin infection in mice and exhibits antibacterial activity by inducing oxidative stress response and cell membrane disintegration in macrophages, Nanomedicine Nanotechnology, Biol. Med. 10 (2014) 1195–1208. https://doi.org/10.1016/j.nano.2014.02.012
[82] A.K. Barui, S.K. Nethi, C.R. Patra, Investigation of the role of nitric oxide driven angiogenesis by zinc oxide nanoflowers, J. Mater. Chem. B. 5 (2017) 3391–3403. https://doi.org/10.1039/c6tb03323g
[83] M.A. Shalaby, M.M. Anwar, H. Saeed, Nanomaterials for application in wound Healing: current state-of-the-art and future perspectives, Springer Netherlands, 2022. https://doi.org/10.1007/s10965-021-02870-x
[84] P. Thangavel, R. Kannan, B. Ramachandran, G. Moorthy, L. Suguna, V. Muthuvijayan, Development of reduced graphene oxide (rGO)-isabgol nanocomposite dressings for enhanced vascularization and accelerated wound healing in normal and diabetic rats, Elsevier Inc., 2018. https://doi.org/10.1016/j.jcis.2018.01.110
[85] M. Mitra, C. Kulsi, K. Chatterjee, K. Kargupta, S. Ganguly, D. Banerjee, S. Goswami, Reduced graphene oxide-polyaniline composites – Synthesis, characterization and optimization for thermoelectric applications, RSC Adv. 5 (2015) 31039–31048. https://doi.org/10.1039/c5ra01794g
[86] S. Mohammadi, A. Babaei, Poly (vinyl alcohol)/chitosan/polyethylene glycol-assembled graphene oxide bio-nanocomposites as a prosperous candidate for biomedical applications and drug/food packaging industry, Int. J. Biol. Macromol. 201 (2022) 528–538. https://doi.org/10.1016/j.ijbiomac.2022.01.086
[87] A. Khalid, A. Madni, B. Raza, M. ul Islam, A. Hassan, F. Ahmad, H. Ali, T. Khan, F. Wahid, Multiwalled carbon nanotubes functionalized bacterial cellulose as an efficient healing material for diabetic wounds, Int. J. Biol. Macromol. 203 (2022) 256–267. https://doi.org/10.1016/j.ijbiomac.2022.01.146
[88] C. Zgheib, R. Biology, S.A. Hilton, R. Biology, L.C. Dewberry, R. Biology, M.M. Hodges, R. Biology, S. Ghatak, J. Xu, R. Biology, S. Singh, A.M. Processing, A. Centre, HHS Public Access, 228 (2021) 107–115. https://doi.org/10.1016/j.jamcollsurg.2018.09.017.Use
[89] K. Viswanathan, D.B. Babu, G. Jayakumar, G. Dhinakar Raj, Anti-microbial and skin wound dressing application of molecular iodine nanoparticles, Mater. Res. Express. 4 (2017) 104003. https://doi.org/10.1088/2053-1591/aa91e5
[90] B. Ma, W. Dang, Z. Yang, J. Chang, C. Wu, MoS2 Nanoclusters-based biomaterials for disease- impaired wound therapy, Appl. Mater. Today. 20 (2020) 100735. https://doi.org/10.1016/j.apmt.2020.100735
[91] A. Samadi, J. Buro, X. Dong, A. Weinstein, D.O. Lara, K.B. Celie, M.A. Wright, M.A. Gadijko, U. Galili, J.A. Spector, Topical α-Gal Nanoparticles Enhance Wound Healing in Radiated Skin, Skin Pharmacol. Physiol. 35 (2022) 31–40. https://doi.org/10.1159/000518015
[92] R. Sankar, R. Dhivya, K.S. Shivashangari, V. Ravikumar, Wound healing activity of Origanum vulgare engineered titanium dioxide nanoparticles in Wistar Albino rats, J. Mater. Sci. Mater. Med. 25 (2014) 1701–1708. https://doi.org/10.1007/s10856-014-5193-5
[93] L. Houdaille, G. Prévot, H. Ripault, J.Y. Lemonnier, C. Réa, D. Chavanne, J.B. Gauvain, Miliary tuberculosis with crystal deposition disease leading to a diagnosis of tuberculous arthritis [1], Jt. Bone Spine. 69 (2002) 338–340. https://doi.org/10.1016/S1297-319X(02)00405-0
[94] S.P. Ndlovu, K. Ngece, S. Alven, B.A. Aderibigbe, Gelatin-based hybrid scaffolds: Promising wound dressings, Polymers (Basel). 13 (2021). https://doi.org/10.3390/polym13172959
[95] T. de P. de L. Lima, M.F. Passos, Skin wounds, the healing process, and hydrogel-based wound dressings: a short review, J. Biomater. Sci. Polym. Ed. 32 (2021) 1910–1925. https://doi.org/10.1080/09205063.2021.1946461
[96] A.G. Niculescu, A.M. Grumezescu, An Up-to-Date Review of Biomaterials Application in Wound Management, Polymers (Basel). 14 (2022) 1–24. https://doi.org/10.3390/polym14030421
[97] H.M. Powell, S.T. Boyce, Fiber density of electrospun gelatin scaffolds regulates morphogenesis of dermal-epidermal skin substitutes, J. Biomed. Mater. Res. – Part A. 84 (2008) 1078–1086. https://doi.org/10.1002/jbm.a.31498
[98] H. Bilgic, M. Demiriz, M. Ozler, T. Ide, N. Dogan, S. Gumus, A. Kiziltay, T. Endogan, V. Hasirci, N. Hasirci, Gelatin based scaffolds and effect of EGF dose on wound healing, J. Biomater. Tissue Eng. 3 (2013) 205–211. https://doi.org/10.1166/jbt.2013.1077
[99] H. Ye, J. Cheng, K. Yu, In situ reduction of silver nanoparticles by gelatin to obtain porous silver nanoparticle/chitosan composites with enhanced antimicrobial and wound-healing activity, Elsevier B.V, 2019. https://doi.org/10.1016/j.ijbiomac.2018.10.056
[100] T.D. Nguyen, T.T. Nguyen, K.L. Ly, A.H. Tran, T.T.N. Nguyen, M.T. Vo, H.M. Ho, N.T.N. Dang, V.T. Vo, D.H. Nguyen, T.T.H. Nguyen, T.H. Nguyen, In vivo study of the antibacterial chitosan/polyvinyl alcohol loaded with silver nanoparticle hydrogel for wound healing applications, Int. J. Polym. Sci. 2019 (2019). https://doi.org/10.1155/2019/7382717
[101] D. Xiang, X. Wu, W. Cao, B. Xue, M. Qin, Y. Cao, W. Wang, Hydrogels With Tunable Mechanical Properties Based on Photocleavable Proteins, Front. Chem. 8 (2020) 1–9. https://doi.org/10.3389/fchem.2020.00007
[102] G. Patil, R. Pawar, S. Jadhav, V. Ghormade, A chitosan based multimodal “soft” hydrogel for rapid hemostasis of non-compressible hemorrhages and its mode of action, Carbohydr. Polym. Technol. Appl. 4 (2022) 100237. https://doi.org/10.1016/j.carpta.2022.100237
[103] J.V. Kumbhar, J.M. Rajwade, K.M. Paknikar, Fruit peels support higher yield and superior quality bacterial cellulose production, Appl. Microbiol. Biotechnol. 99 (2015) 6677–6691. https://doi.org/10.1007/s00253-015-6644-8
[104] H. Moradpoor, H. Mohammadi, M. Safaei, H.R. Mozaffari, R. Sharifi, P. Gorji, A.B. Sulong, N. Muhamad, M. Ebadi, Recent Advances on Bacterial Cellulose-Based Wound Management: Promises and Challenges, Int. J. Polym. Sci. 2022 (2022). https://doi.org/10.1155/2022/1214734
[105] J.M. Rajwade, K.M. Paknikar, J. V. Kumbhar, Applications of bacterial cellulose and its composites in biomedicine, Appl. Microbiol. Biotechnol. 99 (2015) 2491–2511. https://doi.org/10.1007/s00253-015-6426-3
[106] A. Fallacara, E. Baldini, S. Manfredini, S. Vertuani, Hyaluronic acid in the third millennium, Polymers (Basel). 10 (2018). https://doi.org/10.3390/polym10070701
[107] A.M. Abdel-Mohsen, J. Jancar, R.M. Abdel-Rahman, L. Vojtek, P. Hyršl, M. Dušková, H. Nejezchlebová, A novel in situ silver/hyaluronan bio-nanocomposite fabrics for wound and chronic ulcer dressing: In vitro and in vivo evaluations, Int. J. Pharm. 520 (2017) 241–253. https://doi.org/10.1016/j.ijpharm.2017.02.003
[108] K.M. Paknikar, Therapeutic applications of silver nanoparticles, in: Appl. Nanomater., 2013
[109] H. Kenar, C.Y. Ozdogan, C. Dumlu, E. Doger, G.T. Kose, V. Hasirci, Microfibrous scaffolds from poly(L-lactide-co-ε-caprolactone) blended with xeno-free collagen/hyaluronic acid for improvement of vascularization in tissue engineering applications, Mater. Sci. Eng. C. 97 (2019) 31–44. https://doi.org/10.1016/j.msec.2018.12.011
[110] M. Parani, G. Lokhande, A. Singh, A.K. Gaharwar, Engineered Nanomaterials for Infection Control and Healing Acute and Chronic Wounds, ACS Appl. Mater. Interfaces. 8 (2016) 10049–10069. https://doi.org/10.1021/acsami.6b00291
[111] H. Liu, C. Wang, C. Li, Y. Qin, Z. Wang, F. Yang, Z. Li, J. Wang, A functional chitosan-based hydrogel as a wound dressing and drug delivery system in the treatment of wound healing, RSC Adv. 8 (2018) 7533–7549. https://doi.org/10.1039/c7ra13510f
[112] Y. Chen, N. Dan, W. Dan, X. Liu, L. Cong, A novel antibacterial acellular porcine dermal matrix cross-linked with oxidized chitosan oligosaccharide and modified by in situ synthesis of silver nanoparticles for wound healing applications, Mater. Sci. Eng. C. 94 (2019) 1020–1036. https://doi.org/10.1016/j.msec.2018.10.036
[113] S.P. Miguel, A.F. Moreira, I.J. Correia, Chitosan based-asymmetric membranes for wound healing: A review, Int. J. Biol. Macromol. 127 (2019) 460–475. https://doi.org/10.1016/j.ijbiomac.2019.01.072
[114] Z. Bagher, A. Ehterami, M.H. Safdel, H. Khastar, H. Semiari, A. Asefnejad, S.M. Davachi, M. Mirzaii, M. Salehi, Wound healing with alginate/chitosan hydrogel containing hesperidin in rat model, J. Drug Deliv. Sci. Technol. 55 (2020) 101379. https://doi.org/10.1016/j.jddst.2019.101379
[115] T. Takei, H. Nakahara, H. Ijima, K. Kawakami, Synthesis of a chitosan derivative soluble at neutral pH and gellable by freeze-thawing, and its application in wound care, Acta Biomater. 8 (2012) 686–693. https://doi.org/10.1016/j.actbio.2011.10.005
[116] M. Basha, M.M. AbouSamra, G.A. Awad, S.S. Mansy, A potential antibacterial wound dressing of cefadroxil chitosan nanoparticles in situ gel: Fabrication, in vitro optimization and in vivo evaluation, Int. J. Pharm. 544 (2018) 129–140. https://doi.org/10.1016/j.ijpharm.2018.04.021
[117] J. Qu, X. Zhao, Y. Liang, T. Zhang, P.X. Ma, B. Guo, Antibacterial adhesive injectable hydrogels with rapid self-healing, extensibility and compressibility as wound dressing for joints skin wound healing, Biomaterials. 183 (2018) 185–199. https://doi.org/10.1016/j.biomaterials.2018.08.044
[118] M.M. Shaik, A. Dapkekar, J.M. Rajwade, S.H. Jadhav, M. Kowshik, Antioxidant-antibacterial containing bi-layer scaffolds as potential candidates for management of oxidative stress and infections in wound healing, J. Mater. Sci. Mater. Med. 30 (2019). https://doi.org/10.1007/s10856-018-6212-8
[119] Y. Gao, Y. Wu, Recent advances of chitosan-based nanoparticles for biomedical and biotechnological applications, Int. J. Biol. Macromol. 203 (2022) 379–388. https://doi.org/10.1016/j.ijbiomac.2022.01.162
[120] J. Grip, R.E. Engstad, I. Skjæveland, N. Škalko-Basnet, J. Isaksson, P. Basnet, A.M. Holsæter, Beta-glucan-loaded nanofiber dressing improves wound healing in diabetic mice, Eur. J. Pharm. Sci. 121 (2018) 269–280. https://doi.org/10.1016/j.ejps.2018.05.031
[121] F. Esa, S.M. Tasirin, N.A. Rahman, Overview of Bacterial Cellulose Production and Application, Agric. Agric. Sci. Procedia. 2 (2014) 113–119. https://doi.org/10.1016/j.aaspro.2014.11.017
[122] M.B. Noremylia, M.Z. Hassan, Z. Ismail, Recent advancement in isolation, processing, characterization and applications of emerging nanocellulose: A review, Int. J. Biol. Macromol. 206 (2022) 954–976. https://doi.org/10.1016/j.ijbiomac.2022.03.064
[123] S. Khan, M. Ul-Islam, M.W. Ullah, Y. Zhu, K.B. Narayanan, S.S. Han, J.K. Park, Fabrication strategies and biomedical applications of three-dimensional bacterial cellulose-based scaffolds: A review, Int. J. Biol. Macromol. 209 (2022) 9–30. https://doi.org/10.1016/j.ijbiomac.2022.03.191
[124] J.D.P. de Amorim, C.J.G. da Silva Junior, A.D.M. de Medeiros, H.A. do Nascimento, M. Sarubbo, T.P.M. de Medeiros, A.F. de S. Costa, L.A. Sarubbo, Bacterial Cellulose as a Versatile Biomaterial for Wound Dressing Application, Molecules. 27 (2022). https://doi.org/10.3390/molecules27175580
[125] F. Jabbari, V. Babaeipour, S. Bakhtiari, Bacterial cellulose-based composites for nerve tissue engineering, Int. J. Biol. Macromol. 217 (2022) 120–130. https://doi.org/10.1016/j.ijbiomac.2022.07.037
[126] M.M.P. Silva, M.I.F. de Aguiar, A.B. Rodrigues, M.D.C. Miranda, M.Â.M. Araújo, I.L.T.P. Rolim, A.M.A. e Souza, The use of nanoparticles in wound treatment: A systematic review, Rev. Da Esc. Enferm. 51 (2017) 1–9. https://doi.org/10.1590/S1980-220X2016043503272
[127] B. Wang, P. Ji, Y. Ma, J. Song, Z. You, S. Chen, Bacterial cellulose nanofiber reinforced poly(glycerol-sebacate) biomimetic matrix for 3D cell culture, Cellulose. 28 (2021) 8483–8492. https://doi.org/10.1007/s10570-021-04053-9
[128] J. Cai, J. Chen, Q. Zhang, M. Lei, J. He, A. Xiao, C. Ma, S. Li, H. Xiong, Well-aligned cellulose nanofiber-reinforced polyvinyl alcohol composite film: Mechanical and optical properties, Carbohydr. Polym. 140 (2016) 238–245. https://doi.org/10.1016/j.carbpol.2015.12.039
[129] E. Liyaskina, V. Revin, E. Paramonova, M. Nazarkina, N. Pestov, N. Revina, S. Kolesnikova, Nanomaterials from bacterial cellulose for antimicrobial wound dressing, J. Phys. Conf. Ser. 784 (2017) 012034. https://doi.org/10.1088/1742-6596/784/1/012034
[130] M. Moniri, A.B. Moghaddam, S. Azizi, R.A. Rahim, S.W. Zuhainis, M. Navaderi, R. Mohamad, In vitro molecular study of wound healing using biosynthesized bacteria nanocellulose/ silver nanocomposite assisted by bioinformatics databases, Int. J. Nanomedicine. 13 (2018) 5097–5112. https://doi.org/10.2147/IJN.S164573
[131] T.I. Shaheen, I. Capron, Formulation of re-dispersible dry o/w emulsions using cellulose nanocrystals decorated with metal/metal oxide nanoparticles, RSC Adv. 11 (2021) 32143–32151. https://doi.org/10.1039/d1ra06054f
[132] A. Rojewska, A. Karewicz, K. Boczkaja, K. Wolski, M. Kępczyński, S. Zapotoczny, M. Nowakowska, Modified bionanocellulose for bioactive wound-healing dressing, Eur. Polym. J. 96 (2017) 200–209. https://doi.org/10.1016/j.eurpolymj.2017.09.010
[133] R. Portela, C.R. Leal, P.L. Almeida, R.G. Sobral, Bacterial cellulose: a versatile biopolymer for wound dressing applications, Microb. Biotechnol. 12 (2019) 586–610. https://doi.org/10.1111/1751-7915.13392
[134] W.K. Czaja, D.J. Young, M. Kawecki, R.M. Brown, The future prospects of microbial cellulose in biomedical applications, Biomacromolecules. 8 (2007) 1–12. https://doi.org/10.1021/bm060620d
[135] T. Wild, M. Bruckner, M. Payrich, C. Schwarz, T. Eberlein, A. Andriessen, Eradication of methicillin-resistant Staphylococcus aureus in pressure ulcers comparing a polyhexanide-containing cellulose dressing with polyhexanide swabs in a prospective randomized study, Adv. Ski. Wound Care. 25 (2012) 17–22. https://doi.org/10.1097/01.ASW.0000410686.14363.ea
[136] G.F. Picheth, C.L. Pirich, M.R. Sierakowski, M.A. Woehl, C.N. Sakakibara, C.F. de Souza, A.A. Martin, R. da Silva, R.A. de Freitas, Bacterial cellulose in biomedical applications: A review, Int. J. Biol. Macromol. 104 (2017) 97–106. https://doi.org/10.1016/j.ijbiomac.2017.05.171
[137] W. Wang, H. Sheng, D. Cao, F. Zhang, W. Zhang, F. Yan, D. Ding, N. Cheng, S-nitrosoglutathione functionalized polydopamine nanoparticles incorporated into chitosan/gelatin hydrogel films with NIR-controlled photothermal/NO-releasing therapy for enhanced wound healing, Int. J. Biol. Macromol. 200 (2022) 77–86. https://doi.org/10.1016/j.ijbiomac.2021.12.125
[138] B. Blanco-Fernandez, O. Castaño, M.Á. Mateos-Timoneda, E. Engel, S. Pérez-Amodio, Nanotechnology Approaches in Chronic Wound Healing, Adv. Wound Care. 10 (2021) 234–256. https://doi.org/10.1089/wound.2019.1094
[139] N. Hadrup, A.K. Sharma, K. Loeschner, Toxicity of silver ions, metallic silver, and silver nanoparticle materials after in vivo dermal and mucosal surface exposure: A review, Regul. Toxicol. Pharmacol. 98 (2018) 257–267. https://doi.org/10.1016/j.yrtph.2018.08.007
[140] A. Ali, M. Suhail, S. Mathew, M.A. Shah, S.M. Harakeh, S. Ahmad, Z. Kazmi, M.A.R. Alhamdan, A. Chaudhary, G.A. Damanhouri, I. Qadri, Nanomaterial induced immune responses and cytotoxicity, J. Nanosci. Nanotechnol. 16 (2016) 40–57. https://doi.org/10.1166/jnn.2016.10885
[141] K. Sooklert, S. Nilyai, R. Rojanathanes, D. Jindatip, N. Sae-Liang, N. Kitkumthorn, A. Mutirangura, A. Sereemaspun, N-acetylcysteine reverses the decrease of DNA methylation status caused by engineered gold, silicon, and chitosan nanoparticles, Int. J. Nanomedicine. 14 (2019) 4573–4587. https://doi.org/10.2147/IJN.S204372
[142] N.C. da R. Galucio, D. de A. Moysés, J.R.S. Pina, P.S.B. Marinho, P.C. Gomes Júnior, J.N. Cruz, V.V. Vale, A.S. Khayat, A.M. do R. Marinho, Antiproliferative, genotoxic activities and quantification of extracts and cucurbitacin B obtained from Luffa operculata (L.) Cogn, Arab. J. Chem. 15 (2022) 103589. https://doi.org/10.1016/j.arabjc.2021.103589
[143] M. Walker, C.A. Cochrane, P.G. Bowler, D. Parsons, P. Bradshaw, Silver deposition and tissue staining associated with wound dressings containing silver, Ostomy Wound Manag. 52 (2006) 42–50
[144] B.C. Palmer, S.J. Phelan-Dickenson, L.A. Delouise, Multi-walled carbon nanotube oxidation dependent keratinocyte cytotoxicity and skin inflammation, Part. Fibre Toxicol. 16 (2019) 1–16. https://doi.org/10.1186/s12989-018-0285-x
[145] S. Hashempour, S. Ghanbarzadeh, H.I. Maibach, M. Ghorbani, H. Hamishehkar, Skin toxicity of topically applied nanoparticles, Ther. Deliv. 10 (2019) 383–396. https://doi.org/10.4155/tde-2018-0060
[146] C.M.A. Rego, A.F. Francisco, C.N. Boeno, M. V. Paloschi, J.A. Lopes, M.D.S. Silva, H.M. Santana, S.N. Serrath, J.E. Rodrigues, C.T.L. Lemos, R.S.S. Dutra, J.N. da Cruz, C.B.R. dos Santos, S. da S. Setúbal, M.R.M. Fontes, A.M. Soares, W.L. Pires, J.P. Zuliani, Inflammasome NLRP3 activation induced by Convulxin, a C-type lectin-like isolated from Crotalus durissus terrificus snake venom, Sci. Rep. 12 (2022) 1–17. https://doi.org/10.1038/s41598-022-08735-7
[147] I. Barros Almeida, L. Garcez Barretto Teixeira, F. Oliveira De Carvalho, É. Ramos Silva, P. Santos Nunes, M.R. Viana Dos Santos, A. Antunes De Souza Araújo, Smart dressings for wound healing: A review, Adv. Ski. Wound Care. 34 (2021) 1–8. https://doi.org/10.1097/01.ASW.0000725188.95109.68