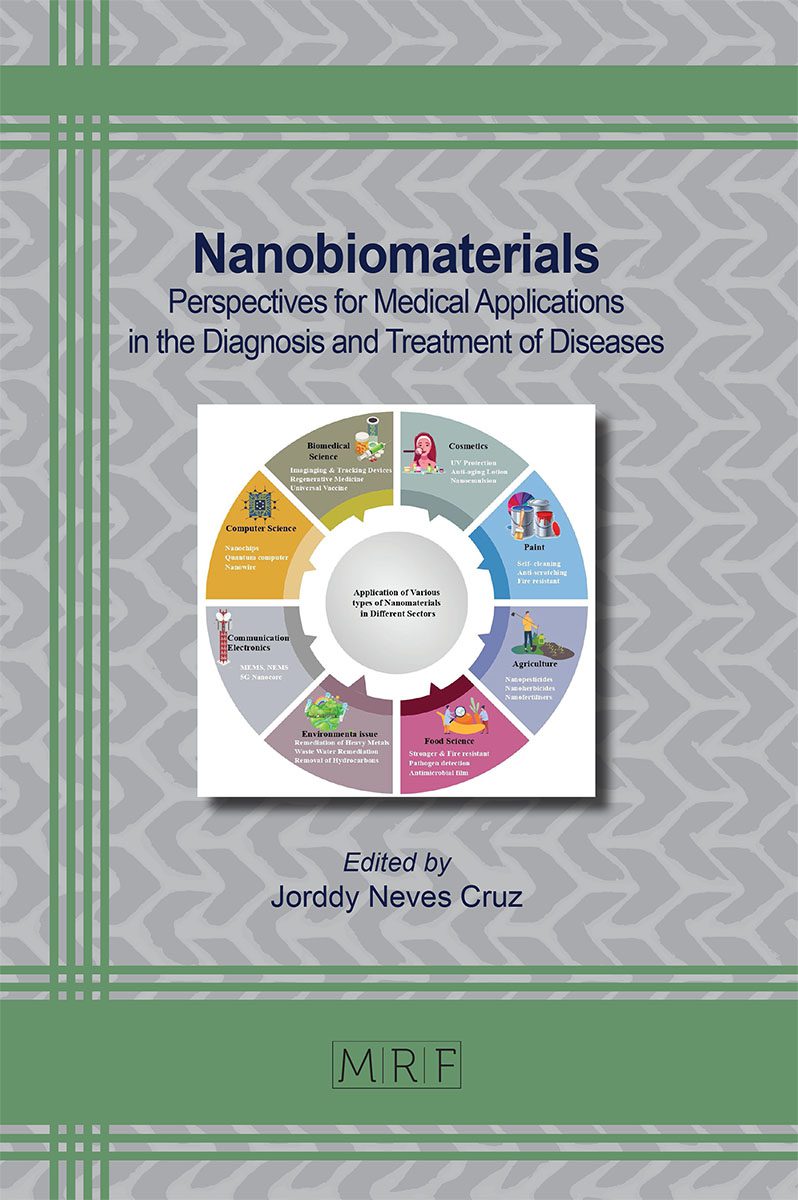
Applications of Nanomaterials in Cancer Diagnosis
Syeda Mariam Fatima, Usman Ali Ashfaq, Muhammad Qasim, Sehar Aslam, Samman Munir, Muhammad Hassan Sarfraz, Muhammad Bilal, Mohsin Khurshid
The early detection of cancer is extremely important in the fight against cancer. However, the detection of various cancers in their early stages has been impeded by the inherent capacity of conventional diagnostic methods. Nanotechnology has provided new materials and contrast agents for an earlier and more accurate diagnosis of cancers as well as the prognosis of cancers during cancer treatment. Therefore, it is believed that nanotechnology could provide a highly sensitive, specific, and multiplexed capacity to measure extracellular cancer biomarkers and can be able to detect cancer cells. In this chapter, the recent developments in the application of nanotechnology for the diagnosis of cancers have been summarized. Further, the key issues which hinder the clinical application of nanotechnology-based diagnostic approaches have been discussed.
Keywords
Biomarkers, Cancer, Ultrasound, Imaging, Diagnosis, Prognosis
Published online , 31 pages
Citation: Syeda Mariam Fatima, Usman Ali Ashfaq, Muhammad Qasim, Sehar Aslam, Samman Munir, Muhammad Hassan Sarfraz, Muhammad Bilal, Mohsin Khurshid, Applications of Nanomaterials in Cancer Diagnosis, Materials Research Proceedings, Vol. 145, pp 250-280, 2023
DOI: https://doi.org/10.21741/9781644902370-10
Part of the book on Nanobiomaterials
References
[1] A. Rezaianzadeh, M. Jalali, A. Maghsoudi, A.M. Mokhtari, S.H. Azgomi, S.L. Dehghani, The overall 5-year survival rate of breast cancer among Iranian women: A systematic review and meta-Analysis of published studies, Breast Dis. 37 (2017) 63–68. https://doi.org/10.3233/BD-160244
[2] S. Bhatia, J. V. Frangioni, R.M. Hoffman, A.J. Iafrate, K. Polyak, The challenges posed by cancer heterogeneity, Nat. Biotechnol. 30 (2012) 604–610. https://doi.org/10.1038/nbt.2294
[3] D. Dornan, J. Settleman, Dissecting cancer heterogeneity, Nat. Biotechnol. 29 (2011) 1095–1096. https://doi.org/10.1038/nbt.2063
[4] N.C. da R. Galucio, D. de A. Moysés, J.R.S. Pina, P.S.B. Marinho, P.C. Gomes Júnior, J.N. Cruz, V.V. Vale, A.S. Khayat, A.M. do R. Marinho, Antiproliferative, genotoxic activities and quantification of extracts and cucurbitacin B obtained from Luffa operculata (L.) Cogn, Arab. J. Chem. 15 (2022) 103589. https://doi.org/10.1016/j.arabjc.2021.103589
[5] R. Zeineldin, Nanotechnology for cancer screening and diagnosis: from innovations to clinical applications, Biomater. Cancer Ther. (2020) 261–289. https://doi.org/10.1016/b978-0-08-102983-1.00010-7
[6] Y.E. Choi, J.W. Kwak, J.W. Park, Nanotechnology for early cancer detection, Sensors. 10 (2010) 428–455. https://doi.org/10.3390/s100100428
[7] A.B. Chinen, C.M. Guan, J.R. Ferrer, S.N. Barnaby, T.J. Merkel, C.A. Mirkin, Nanoparticle Probes for the Detection of Cancer Biomarkers, Cells, and Tissues by Fluorescence, Chem. Rev. 115 (2015) 10530–10574. https://doi.org/10.1021/acs.chemrev.5b00321
[8] S. Jia, R. Zhang, Z. Li, J. Li, Clinical and biological significance of circulating tumor cells, circulating tumor DNA, and exosomes as biomarkers in colorectal cancer, Oncotarget. 8 (2017) 55632–55645. https://doi.org/10.18632/oncotarget.17184
[9] X.J. Chen, X.Q. Zhang, Q. Liu, J. Zhang, G. Zhou, Nanotechnology: A promising method for oral cancer detection and diagnosis, J. Nanobiotechnology. 16 (2018) 52. https://doi.org/10.1186/s12951-018-0378-6
[10] T.L. Doane, C. Burda, The unique role of nanoparticles in nanomedicine: Imaging, drug delivery and therapy, Chem. Soc. Rev. 41 (2012) 2885–2911. https://doi.org/10.1039/c2cs15260f
[11] J.R. Lakowicz, Radiative decay engineering 5: Metal-enhanced fluorescence and plasmon emission, Anal. Biochem. 337 (2005) 171–194. https://doi.org/10.1016/j.ab.2004.11.026
[12] M. Schmelzeisen, Y. Zhao, M. Klapper, K. Müllen, M. Kreiter, Fluorescence enhancement from individual plasmonic gap resonances, ACS Nano. 4 (2010) 3309–3317. https://doi.org/10.1021/nn901655v
[13] A.S. Thakor, J. Jokerst, C. Zavaleta, T.F. Massoud, S.S. Gambhir, Gold nanoparticles: A revival in precious metal administration to patients, Nano Lett. 11 (2011) 4029–4036. https://doi.org/10.1021/nl202559p
[14] D. Pan, M. Pramanik, S.A. Wickline, L. V. Wang, G.M. Lanza, Recent advances in colloidal gold nanobeacons for molecular photoacoustic imaging, Contrast Media Mol. Imaging. 6 (2011) 378–388. https://doi.org/10.1002/cmmi.449
[15] W.J. Akers, C. Kim, M. Berezin, K. Guo, R. Fuhrhop, G.M. Lanza, G.M. Fischer, E. Daltrozzo, A. Zumbusch, X. Cai, L. V. Wang, S. Achilefu, Noninvasive photoacoustic and fluorescence sentinel lymph node identification using dye-loaded perfluorocarbon nanoparticles, ACS Nano. 5 (2011) 173–182. https://doi.org/10.1021/nn102274q
[16] M. Bruchez, M. Moronne, P. Gin, S. Weiss, A.P. Alivisatos, Semiconductor nanocrystals as fluorescent biological labels, Science (80-. ). 281 (1998) 2013–2016. https://doi.org/10.1126/science.281.5385.2013
[17] K.E. Sapsford, T. Pons, I.L. Medintz, H. Mattoussi, Biosensing with luminescent semiconductor quantum dots, Sensors. 6 (2006) 925–953. https://doi.org/10.3390/s6080925
[18] R. Antiochia, P. Bollella, G. Favero, F. Mazzei, Nanotechnology-Based Surface Plasmon Resonance Affinity Biosensors for in Vitro Diagnostics, Int. J. Anal. Chem. 2016 (2016) 2981931. https://doi.org/10.1155/2016/2981931
[19] P. Abdul Rasheed, N. Sandhyarani, Quartz crystal microbalance genosensor for sequence specific detection of attomolar DNA targets, Anal. Chim. Acta. 905 (2016) 134–139. https://doi.org/10.1016/j.aca.2015.11.033
[20] M. Medina-Sánchez, S. Miserere, A. Merkoçi, Nanomaterials and lab-on-a-chip technologies, Lab Chip. 12 (2012) 1932–1943. https://doi.org/10.1039/c2lc40063d
[21] C.H. Vannoy, A.J. Tavares, M. Omair Noor, U. Uddayasankar, U.J. Krull, Biosensing with quantum dots: A microfluidic approach, Sensors. 11 (2011) 9732–9763. https://doi.org/10.3390/s111009732
[22] A.A. Ghazani, J.A. Lee, J. Klostranec, Q. Xiang, R.S. Dacosta, B.C. Wilson, M.S. Tsao, W.C.W. Chan, High throughput quantification of protein expression of cancer antigens in tissue microarray using quantum dot nanocrystals, Nano Lett. 6 (2006) 2881–2886. https://doi.org/10.1021/nl062111n
[23] S.W. Dutse, N.A. Yusof, Microfluidics-based lab-on-chip systems in DNA-based biosensing: An overview, Sensors. 11 (2011) 5754–5768. https://doi.org/10.3390/s110605754
[24] L. Wang, P.C.H. Li, Microfluidic DNA microarray analysis: A review, Anal. Chim. Acta. 687 (2011) 12–27. https://doi.org/10.1016/j.aca.2010.11.056
[25] S.J. Maerkl, Next generation microfluidic platforms for high-throughput protein biochemistry, Curr. Opin. Biotechnol. 22 (2011) 59–65. https://doi.org/10.1016/j.copbio.2010.08.010
[26] C.S. Thaxton, D.G. Georganopoulou, C.A. Mirkin, Gold nanoparticle probes for the detection of nucleic acid targets, Clin. Chim. Acta. 363 (2006) 120–126. https://doi.org/10.1016/j.cccn.2005.05.042
[27] M. Tagliazucchi, M.G. Blaber, G.C. Schatz, E.A. Weiss, I. Szleifer, Optical properties of responsive hybrid Au@polymer nanoparticles, ACS Nano. 6 (2012) 8397–8406. https://doi.org/10.1021/nn303221y
[28] S. Rana, A.K. Singla, A. Bajaj, S.G. Elci, O.R. Miranda, R. Mout, B. Yan, F.R. Jirik, V.M. Rotello, Array-based sensing of metastatic cells and tissues using nanoparticle-fluorescent protein conjugates, ACS Nano. 6 (2012) 8233–8240. https://doi.org/10.1021/nn302917e
[29] S. Chemburu, K. Fenton, G.P. Lopez, R. Zeineldin, Biomimetic silica microspheres in biosensing, Molecules. 15 (2010) 1932–1957. https://doi.org/10.3390/molecules15031932
[30] D. Issadore, C. Min, M. Liong, J. Chung, R. Weissleder, H. Lee, Miniature magnetic resonance system for point-of-care diagnostics, Lab Chip. 11 (2011) 2282–2287. https://doi.org/10.1039/c1lc20177h
[31] J.B. Haun, T.J. Yoon, H. Lee, R. Weissleder, Molecular detection of biomarkers and cells using magnetic nanoparticles and diagnostic magnetic resonance, Methods Mol. Biol. 726 (2011) 33–49. https://doi.org/10.1007/978-1-61779-052-2_3
[32] X. Sun, D. Ho, L.M. Lacroix, J.Q. Xiao, S. Sun, Magnetic nanoparticles for magnetoresistance-based biodetection, IEEE Trans. Nanobioscience. 11 (2012) 46–53. https://doi.org/10.1109/TNB.2011.2176509
[33] B.N. Johnson, R. Mutharasan, Biosensing using dynamic-mode cantilever sensors: A review, Biosens. Bioelectron. 32 (2012) 1–18. https://doi.org/10.1016/j.bios.2011.10.054
[34] F. Huber, H.P. Lang, J. Zhang, D. Rimoldi, C. Gerber, Nanosensors for cancer detection, Swiss Med. Wkly. 145 (2015). https://doi.org/10.4414/smw.2015.14092
[35] N. Triroj, P. Jaroenapibal, H. Shi, J.I. Yeh, R. Beresford, Microfluidic chip-based nanoelectrode array as miniaturized biochemical sensing platform for prostate-specific antigen detection, Biosens. Bioelectron. 26 (2011) 2927–2933. https://doi.org/10.1016/j.bios.2010.11.039
[36] S. Viswanathan, C. Rani, S. Ribeiro, C. Delerue-Matos, Molecular imprinted nanoelectrodes for ultra sensitive detection of ovarian cancer marker, Biosens. Bioelectron. 33 (2012) 179–183. https://doi.org/10.1016/j.bios.2011.12.049
[37] J.R. Chevillet, I. Lee, H.A. Briggs, Y. He, K. Wang, Issues and prospects of microRNA-based biomarkers in blood and other body fluids, Molecules. 19 (2014) 6080–6105. https://doi.org/10.3390/molecules19056080
[38] H. Ma, J. Liu, M.M. Ali, M.A.I. Mahmood, L. Labanieh, M. Lu, S.M. Iqbal, Q. Zhang, W. Zhao, Y. Wan, Nucleic acid aptamers in cancer research, diagnosis and therapy, Chem. Soc. Rev. 44 (2015) 1240–1256. https://doi.org/10.1039/c4cs00357h
[39] C.A.K. Borrebaeck, Precision diagnostics: Moving towards protein biomarker signatures of clinical utility in cancer, Nat. Rev. Cancer. 17 (2017) 199–204. https://doi.org/10.1038/nrc.2016.153
[40] L.C. Hull, D. Farrell, P. Grodzinski, Highlights of recent developments and trends in cancer nanotechnology research-view from NCI alliance for nanotechnology in cancer, Biotechnol. Adv. 32 (2014) 666–678. https://doi.org/10.1016/j.biotechadv.2013.08.003
[41] M. Sharifi, M.R. Avadi, F. Attar, F. Dashtestani, H. Ghorchian, S.M. Rezayat, A.A. Saboury, M. Falahati, Cancer diagnosis using nanomaterials based electrochemical nanobiosensors, Biosens. Bioelectron. 126 (2019) 773–784. https://doi.org/10.1016/j.bios.2018.11.026
[42] H. Zhang, J. Lv, Z. Jia, Efficient fluorescence resonance energy transfer between quantum dots and gold nanoparticles based on porous silicon photonic crystal for DNA detection, Sensors (Switzerland). 17 (2017) 1–12. https://doi.org/10.3390/s17051078
[43] I.L. Medintz, H.T. Uyeda, E.R. Goldman, H. Mattoussi, Quantum dot bioconjugates for imaging, labelling and sensing, Nat. Mater. 4 (2005) 435–446. https://doi.org/10.1038/nmat1390
[44] R. Freeman, I. Willner, Optical molecular sensing with semiconductor quantum dots (QDs), Chem. Soc. Rev. 41 (2012) 4067–4085. https://doi.org/10.1039/c2cs15357b
[45] V. Anagnostou, K.N. Smith, P.M. Forde, N. Niknafs, R. Bhattacharya, J. White, T. Zhang, V. Adleff, J. Phallen, N. Wali, C. Hruban, V.B. Guthrie, K. Rodgers, J. Naidoo, H. Kang, W. Sharfman, C. Georgiades, F. Verde, P. Illei, Q.K. Li, E. Gabrielson, M. V. Brock, C.A. Zahnow, S.B. Baylin, R.B. Scharpf, J.R. Brahmer, R. Karchin, D.M. Pardoll, V.E. Velculescu, Evolution of neoantigen landscape during immune checkpoint blockade in non-small cell lung cancer, Cancer Discov. 7 (2017) 264–276. https://doi.org/10.1158/2159-8290.CD-16-0828
[46] H. Li, Z. Cao, Y. Zhang, C. Lau, J. Lu, Simultaneous detection of two lung cancer biomarkers using dual-color fluorescence quantum dots, Analyst. 136 (2011) 1399–1405. https://doi.org/10.1039/c0an00704h
[47] B. Gu, C. Xu, C. Yang, S. Liu, M. Wang, ZnO quantum dot labeled immunosensor for carbohydrate antigen 19-9, Biosens. Bioelectron. 26 (2011) 2720–2723. https://doi.org/10.1016/j.bios.2010.09.031
[48] C. Puig-Saus, L.A. Rojas, E. Laborda, A. Figueras, R. Alba, C. Fillat, R. Alemany, IRGD tumor-penetrating peptide-modified oncolytic adenovirus shows enhanced tumor transduction, intratumoral dissemination and antitumor efficacy, Gene Ther. 21 (2014) 767–774. https://doi.org/10.1038/gt.2014.52
[49] R. Tong, V.J. Coyle, L. Tang, A.M. Barger, T.M. Fan, J. Cheng, Polylactide nanoparticles containing stably incorporated cyanine dyes for in vitro and in vivo imaging applications, Microsc. Res. Tech. 73 (2010) 901–909. https://doi.org/10.1002/jemt.20824
[50] M.C. Schwaederlé, S.P. Patel, H. Husain, M. Ikeda, R.B. Lanman, K.C. Banks, A.A. Talasaz, L. Bazhenova, R. Kurzrock, Utility of genomic assessment of blood-derived circulating tumor DNA (ctDNA) in patients with advanced lung adenocarcinoma, Clin. Cancer Res. 23 (2017) 5101–5111. https://doi.org/10.1158/1078-0432.CCR-16-2497
[51] S.J. Tan, T. Yeo, S.A. Sukhatme, S.L. Kong, W.T. Lim, C.T. Lim, Personalized treatment through detection and monitoring of genetic aberrations in single circulating tumor cells, Adv. Exp. Med. Biol. 994 (2017) 255–273. https://doi.org/10.1007/978-3-319-55947-6_14
[52] R. Mehra, S.A. Tomlins, J. Yu, X. Cao, L. Wang, A. Menon, M.A. Rubin, K.J. Pienta, R.B. Shah, A.M. Chinnaiyan, Characterization of TMPRSS2-ETS gene aberrations in androgen-independent metastatic prostate cancer, Cancer Res. 68 (2008) 3584–3590. https://doi.org/10.1158/0008-5472.CAN-07-6154
[53] A.F.J. Jou, C.H. Lu, Y.C. Ou, S.S. Wang, S.L. Hsu, I. Willner, J.A.A. Ho, Diagnosing the miR-141 prostate cancer biomarker using nucleic acid-functionalized CdSe/ZnS QDs and telomerase, Chem. Sci. 6 (2015) 659–665. https://doi.org/10.1039/c4sc02104e
[54] J. Ko, N. Bhagwat, T. Black, S.S. Yee, Y.J. Na, S. Fisher, J. Kim, E.L. Carpenter, B.Z. Stanger, D. Issadore, MiRNA profiling of magnetic nanopore-isolated extracellular vesicles for the diagnosis of pancreatic cancer, Cancer Res. 78 (2018) 3688–3697. https://doi.org/10.1158/0008-5472.CAN-17-3703
[55] Y. Jiang, M. Shi, Y. Liu, S. Wan, C. Cui, L. Zhang, W. Tan, Aptamer/AuNP Biosensor for Colorimetric Profiling of Exosomal Proteins, Angew. Chemie – Int. Ed. 56 (2017) 11916–11920. https://doi.org/10.1002/anie.201703807
[56] T.L. Edwards, C. Giezen, C.M. Browne, Influences of indication response requirement and target prevalence on dogs’ performance in a scent-detection task, Appl. Anim. Behav. Sci. 253 (2022) 105657. https://doi.org/10.1016/j.applanim.2022.105657
[57] T. Jezierski, M. Walczak, T. Ligor, J. Rudnicka, B. Buszewski, Study of the art: Canine olfaction used for cancer detection on the basis of breath odour. Perspectives and limitations, J. Breath Res. 9 (2015) 27001. https://doi.org/10.1088/1752-7155/9/2/027001
[58] A. Krilaviciute, J.A. Heiss, M. Leja, J. Kupcinskas, H. Haick, H. Brenner, Detection of cancer through exhaled breath: A systematic review, Oncotarget. 6 (2015) 38643–38657. https://doi.org/10.18632/oncotarget.5938
[59] K. Ranjan, R. Singh, Dog Nose to E-Nose in Disease Diagnosis, J. Adv. Biol. 11 (2018) 2294–2306. https://doi.org/10.24297/jab.v11i0.7959
[60] Diagnosis and Classification of 17 Diseases from 1404 Subjects via Pattern Analysis of Exhaled Molecules-Supporting Information, (2009) 198–201. https://doi.org/10.1021/acsnano.6b04930.s001
[61] R. Fiammengo, Can nanotechnology improve cancer diagnosis through miRNA detection?, Biomark. Med. 11 (2017) 69–86. https://doi.org/10.2217/bmm-2016-0195
[62] M.P. McRae, G. Simmons, J.T. McDevitt, Challenges and opportunities for translating medical microdevices: Insights from the programmable bio-nano-chip, Bioanalysis. 8 (2016) 905–919. https://doi.org/10.4155/bio-2015-0023
[63] H. Maeda, G.Y. Bharate, J. Daruwalla, Polymeric drugs for efficient tumor-targeted drug delivery based on EPR-effect, Eur. J. Pharm. Biopharm. 71 (2009) 409–419. https://doi.org/10.1016/j.ejpb.2008.11.010
[64] J. Shi, P.W. Kantoff, R. Wooster, O.C. Farokhzad, Cancer nanomedicine: Progress, challenges and opportunities, Nat. Rev. Cancer. 17 (2017) 20–37. https://doi.org/10.1038/nrc.2016.108
[65] J.E. Rosen, L. Chan, D. Bin Shieh, F.X. Gu, Iron oxide nanoparticles for targeted cancer imaging and diagnostics, Nanomedicine Nanotechnology, Biol. Med. 8 (2012) 275–290. https://doi.org/10.1016/j.nano.2011.08.017
[66] L. Fass, Imaging and cancer: A review, Mol. Oncol. 2 (2008) 115–152. https://doi.org/10.1016/j.molonc.2008.04.001
[67] L.M.A. Crane, M. Van Oosten, R.G. Pleijhuis, A. Motekallemi, S.C. Dowdy, W.A. Cliby, A.G.J. Van Der Zee, G.M. Van Dam, Intraoperative imaging in ovarian cancer: Fact or fiction?, Mol. Imaging. 10 (2011) 248–257. https://doi.org/10.2310/7290.2011.00004
[68] H.E.C. Bhang, M.G. Pomper, Cancer imaging: Gene transcription-based imaging and therapeutic systems, Int. J. Biochem. Cell Biol. 44 (2012) 684–689. https://doi.org/10.1016/j.biocel.2012.02.001
[69] I.H. El-Sayed, X. Huang, M.A. El-Sayed, Surface plasmon resonance scattering and absorption of anti-EGFR antibody conjugated gold nanoparticles in cancer diagnostics: Applications in oral cancer, Nano Lett. 5 (2005) 829–834. https://doi.org/10.1021/nl050074e
[70] J.S. Aaron, J. Oh, T.A. Larson, S. Kumar, T.E. Milner, K. V. Sokolov, Increased optical contrast in imaging of epidermal growth factor receptor using magnetically actuated hybrid gold/iron oxide nanoparticles, Opt. Express. 14 (2006) 12930. https://doi.org/10.1364/oe.14.012930
[71] J. V. Jokerst, M. Thangaraj, P.J. Kempen, R. Sinclair, S.S. Gambhir, Photoacoustic imaging of mesenchymal stem cells in living mice via silica-coated gold nanorods, ACS Nano. 6 (2012) 5920–5930. https://doi.org/10.1021/nn302042y
[72] M.B. Dowling, L. Li, J. Park, G. Kumi, A. Nan, H. Ghandehari, J.T. Fourkas, P. Deshong, Multiphoton-absorption-induced-luminescence (MAIL) imaging of tumor-targeted gold nanoparticles, Bioconjug. Chem. 21 (2010) 1968–1977. https://doi.org/10.1021/bc100115m
[73] F. Kiessling, J. Bzyl, S. Fokong, M. Siepmann, G. Schmitz, M. Palmowski, Targeted Ultrasound Imaging of Cancer: An Emerging Technology on its Way to Clinics, Curr. Pharm. Des. 18 (2012) 2184–2199. https://doi.org/10.2174/138161212800099900
[74] J.M. Warram, A.G. Sorace, R. Saini, H.R. Umphrey, K.R. Zinn, K. Hoyt, A triple-targeted ultrasound contrast agent provides improved localization to tumor vasculature, J. Ultrasound Med. 30 (2011) 921–931. https://doi.org/10.7863/jum.2011.30.7.921
[75] A.G. Sorace, R. Saini, M. Mahoney, K. Hoyt, Molecular ultrasound imaging using a targeted contrast agent for assessing early tumor response to antiangiogenic therapy, J. Ultrasound Med. 31 (2012) 1543–1550. https://doi.org/10.7863/jum.2012.31.10.1543
[76] F. Cavalieri, M. Zhou, M. Ashokkumar, The Design of Multifunctional Microbubbles for Ultrasound Image-Guided Cancer Therapy, Curr. Top. Med. Chem. 10 (2010) 1198–1210. https://doi.org/10.2174/156802610791384180
[77] A. de M. Lima, A.S. Siqueira, M.L.S. Möller, R.C. de Souza, J.N. Cruz, A.R.J. Lima, R.C. da Silva, D.C.F. Aguiar, J.L. da S.G.V. Junior, E.C. Gonçalves, In silico improvement of the cyanobacterial lectin microvirin and mannose interaction, J. Biomol. Struct. Dyn. (2020). https://doi.org/10.1080/07391102.2020.1821782
[78] D. Kozlowska, P. Foran, P. MacMahon, M.J. Shelly, S. Eustace, R. O’Kennedy, Molecular and magnetic resonance imaging: The value of immunoliposomes, Adv. Drug Deliv. Rev. 61 (2009) 1402–1411. https://doi.org/10.1016/j.addr.2009.09.003
[79] X.H. Peng, X. Qian, H. Mao, A.Y. Wang, Z.G. Chen, S. Nie, D.M. Shin, Targeted magnetic iron oxide nanoparticles for tumor imaging and therapy, Int. J. Nanomedicine. 3 (2008) 311–321. https://doi.org/10.2147/ijn.s2824
[80] X. Michalet, R. Colyer, J. Antelman, O. Siegmund, A. Tremsin, J. Vallerga, S. Weiss, Single-Quantum Dot Imaging with a Photon Counting Camera, Curr. Pharm. Biotechnol. 10 (2009) 543–557. https://doi.org/10.2174/138920109788922100
[81] M. Longmire, P.L. Choyke, H. Kobayashi, Clearance properties of nano-sized particles and molecules as imaging agents: Considerations and caveats, Nanomedicine. 3 (2008) 703–717. https://doi.org/10.2217/17435889.3.5.703
[82] G. Iyer, X. Michalet, Y.P. Chang, S. Weiss, Tracking Single Proteins in Live Cells Using Single-Chain Antibody Fragment-Fluorescent Quantum Dot Affinity Pair, Methods Enzymol. 475 (2010) 61–79. https://doi.org/10.1016/S0076-6879(10)75003-5
[83] Y. Wang, L. Chen, Quantum dots, lighting up the research and development of nanomedicine, Nanomedicine Nanotechnology, Biol. Med. 7 (2011) 385–402. https://doi.org/10.1016/j.nano.2010.12.006
[84] J.T. Robinson, G. Hong, Y. Liang, B. Zhang, O.K. Yaghi, H. Dai, In vivo fluorescence imaging in the second near-infrared window with long circulating carbon nanotubes capable of ultrahigh tumor uptake, J. Am. Chem. Soc. 134 (2012) 10664–10669. https://doi.org/10.1021/ja303737a
[85] V.J. Pansare, S. Hejazi, W.J. Faenza, R.K. Prud’Homme, Review of long-wavelength optical and NIR imaging materials: Contrast agents, fluorophores, and multifunctional nano carriers, Chem. Mater. 24 (2012) 812–827. https://doi.org/10.1021/cm2028367
[86] H. Kobayashi, M.R. Longmire, M. Ogawa, P.L. Choyke, S. Kawamoto, Multiplexed imaging in cancer diagnosis: Applications and future advances, Lancet Oncol. 11 (2010) 589–595. https://doi.org/10.1016/S1470-2045(10)70009-7
[87] J. Qian, L. Jiang, F. Cai, D. Wang, S. He, Fluorescence-surface enhanced Raman scattering co-functionalized gold nanorods as near-infrared probes for purely optical in vivo imaging, Biomaterials. 32 (2011) 1601–1610. https://doi.org/10.1016/j.biomaterials.2010.10.058
[88] Z. Wang, H. Wu, C. Wang, S. Xu, Y. Cui, Gold aggregates- and quantum dots-embedded nanospheres: Switchable dual-mode image probes for living cells, J. Mater. Chem. 21 (2011) 4307–4313. https://doi.org/10.1039/c0jm03884a
[89] K. Yang, L. Hu, X. Ma, S. Ye, L. Cheng, X. Shi, C. Li, Y. Li, Z. Liu, Multimodal imaging guided photothermal therapy using functionalized graphene nanosheets anchored with magnetic nanoparticles, Adv. Mater. 24 (2012) 1868–1872. https://doi.org/10.1002/adma.201104964
[90] N.M. Rofsky, A.D. Sherry, R.E. Lenkinski, Nephrogenic systemic fibrosis: A chemical perspective, Radiology. 247 (2008) 608–612. https://doi.org/10.1148/radiol.2473071975
[91] A.S. Thakor, J. V. Jokerst, P. Ghanouni, J.L. Campbell, E. Mittra, S.S. Gambhir, Clinically Approved Nanoparticle Imaging Agents, J. Nucl. Med. 57 (2016) 1833–1837. https://doi.org/10.2967/jnumed.116.181362
[92] C.M.A. Rego, A.F. Francisco, C.N. Boeno, M. V. Paloschi, J.A. Lopes, M.D.S. Silva, H.M. Santana, S.N. Serrath, J.E. Rodrigues, C.T.L. Lemos, R.S.S. Dutra, J.N. da Cruz, C.B.R. dos Santos, S. da S. Setúbal, M.R.M. Fontes, A.M. Soares, W.L. Pires, J.P. Zuliani, Inflammasome NLRP3 activation induced by Convulxin, a C-type lectin-like isolated from Crotalus durissus terrificus snake venom, Sci. Rep. 12 (2022) 4706. https://doi.org/10.1038/s41598-022-08735-7
[93] Y. Zhang, M. Li, X. Gao, Y. Chen, T. Liu, Nanotechnology in cancer diagnosis: Progress, challenges and opportunities, J. Hematol. Oncol. 12 (2019) 137. https://doi.org/10.1186/s13045-019-0833-3
[94] J. Youkhanna, J. Syoufjy, M. Rhorer, O. Oladeinde, R. Zeineldin, Toward nanotechnology-based solutions for a particular disease: Ovarian cancer as an example, Nanotechnol. Rev. 2 (2013) 473–484. https://doi.org/10.1515/ntrev-2013-0008
[95] R. Zeineldin, J. Syoufjy, Cancer nanotechnology: Opportunities for prevention, diagnosis, and therapy, Methods Mol. Biol. 1530 (2017) 3–12. https://doi.org/10.1007/978-1-4939-6646-2_1
[96] W. Hong, S. Lee, H.J. Chang, E.S. Lee, Y. Cho, Multifunctional magnetic nanowires: A novel breakthrough for ultrasensitive detection and isolation of rare cancer cells from non-metastatic early breast cancer patients using small volumes of blood, Biomaterials. 106 (2016) 78–86. https://doi.org/10.1016/j.biomaterials.2016.08.020
[97] X. Wu, T. Xiao, Z. Luo, R. He, Y. Cao, Z. Guo, W. Zhang, Y. Chen, A micro-/nano-chip and quantum dots-based 3D cytosensor for quantitative analysis of circulating tumor cells, J. Nanobiotechnology. 16 (2018) 65. https://doi.org/10.1186/s12951-018-0390-x
[98] Q. Huang, F.B. Wang, C.H. Yuan, Z. He, L. Rao, B. Cai, B. Chen, S. Jiang, Z. Li, J. Chen, W. Liu, F. Guo, Z. Ao, S. Chen, X.Z. Zhao, Gelatin nanoparticle-coated silicon beads for density-selective capture and release of heterogeneous circulating tumor cells with high purity, Theranostics. 8 (2018) 1624–1635. https://doi.org/10.7150/thno.23531
[99] N. Sun, X. Li, Z. Wang, R. Zhang, J. Wang, K. Wang, R. Pei, A Multiscale TiO2 Nanorod Array for Ultrasensitive Capture of Circulating Tumor Cells, ACS Appl. Mater. Interfaces. 8 (2016) 12638–12643. https://doi.org/10.1021/acsami.6b02178
[100] C. Wu, T. Schneider, M. Zeigler, J. Yu, P.G. Schiro, D.R. Burnham, J.D. McNeill, D.T. Chiu, Bioconjugation of ultrabright semiconducting polymer dots for specific cellular targeting, J. Am. Chem. Soc. 132 (2010) 15410–15417. https://doi.org/10.1021/ja107196s
[101] J. Shen, K. Li, L. Cheng, Z. Liu, S.T. Lee, J. Liu, Specific detection and simultaneously localized photothermal treatment of cancer cells using layer-by-layer assembled multifunctional nanoparticles, ACS Appl. Mater. Interfaces. 6 (2014) 6443–6452. https://doi.org/10.1021/am405924g
[102] Y. Zhang, B. Chen, M. He, B. Yang, J. Zhang, B. Hu, Immunomagnetic separation combined with inductively coupled plasma mass spectrometry for the detection of tumor cells using gold nanoparticle labeling, Anal. Chem. 86 (2014) 8082–8089. https://doi.org/10.1021/ac500964s
[103] X. Pang, C. Cui, M. Su, Y. Wang, Q. Wei, W. Tan, Construction of self-powered cytosensing device based on ZnO nanodisks@g-C3N4 quantum dots and application in the detection of CCRF-CEM cells, Nano Energy. 46 (2018) 101–109. https://doi.org/10.1016/j.nanoen.2018.01.018
[104] Y. Liu, F. Zhu, W. Dan, Y. Fu, S. Liu, Construction of carbon nanotube based nanoarchitectures for selective impedimetric detection of cancer cells in whole blood, Analyst. 139 (2014) 5086–5092. https://doi.org/10.1039/c4an00758a
[105] C.H. Wu, Y.Y. Huang, P. Chen, K. Hoshino, H. Liu, E.P. Frenkel, J.X.J. Zhang, K. V. Sokolov, Versatile immunomagnetic nanocarrier platform for capturing cancer cells, ACS Nano. 7 (2013) 8816–8823. https://doi.org/10.1021/nn403281e
[106] O. Rabin, J.M. Perez, J. Grimm, G. Wojtkiewicz, R. Weissleder, An X-ray computed tomography imaging agent based on long-circulating bismuth sulphide nanoparticles, Nat. Mater. 5 (2006) 118–122. https://doi.org/10.1038/nmat1571
[107] A. Jakhmola, N. Anton, T.F. Vandamme, Inorganic nanoparticles based contrast agents for X-ray computed tomography, Adv. Healthc. Mater. 1 (2012) 413–431. https://doi.org/10.1002/adhm.201200032
[108] J. Leike, A. Sachse, C. Ehritt, W. Krause, Biodistribution and CT-imaging characteristics of iopromide-carrying liposomes in rats, J. Liposome Res. 6 (1996) 665–680. https://doi.org/10.3109/08982109609039920
[109] Z. Gao, A.M. Kennedy, D.A. Christensen, N.Y. Rapoport, Drug-loaded nano/microbubbles for combining ultrasonography and targeted chemotherapy, Ultrasonics. 48 (2008) 260–270. https://doi.org/10.1016/j.ultras.2007.11.002
[110] J. Bzyl, W. Lederle, A. Rix, C. Grouls, I. Tardy, S. Pochon, M. Siepmann, T. Penzkofer, M. Schneider, F. Kiessling, M. Palmowski, Molecular and functional ultrasound imaging in differently aggressive breast cancer xenografts using two novel ultrasound contrast agents (BR55 and BR38), Eur. Radiol. 21 (2011) 1988–1995. https://doi.org/10.1007/s00330-011-2138-y
[111] M.A. Pysz, K. Foygel, J. Rosenberg, S.S. Gambhir, M. Schneider, J.K. Willmann, Antiangiogenic cancer therapy: Monitoring with molecular US and a clinically translatable contrast agent (BR55), Radiology. 256 (2010) 519–527. https://doi.org/10.1148/radiol.10091858
[112] M.C. Cassidy, H.R. Chan, B.D. Ross, P.K. Bhattacharya, C.M. Marcus, In vivo magnetic resonance imaging of hyperpolarized silicon particles, Nat. Nanotechnol. 8 (2013) 363–368. https://doi.org/10.1038/nnano.2013.65
[113] C. Zhang, M. Jugold, E.C. Woenne, T. Lammers, B. Morgenstern, M.M. Mueller, H. Zentgraf, M. Bock, M. Eisenhut, W. Semmler, F. Kiessling, Specific targeting of tumor angiogenesis by RGD-conjugated ultrasmall superparamagnetic iron oxide particles using a clinical 1.5-T magnetic resonance scanner, Cancer Res. 67 (2007) 1555–1562. https://doi.org/10.1158/0008-5472.CAN-06-1668
[114] P.M. Winter, K. Cai, J. Chen, C.R. Adair, G.E. Kiefer, P.S. Athey, P.J. Gaffney, C.E. Buff, J.D. Robertson, S.D. Caruthers, S.A. Wickline, G.M. Lanza, Targeted PARACEST nanoparticle contrast agent for the detection of fibrin, Magn. Reson. Med. 56 (2006) 1384–1388. https://doi.org/10.1002/mrm.21093
[115] A. Preda, M. Van Vliet, G.P. Krestin, R.C. Brasch, C.F. Van Dijke, Magnetic resonance macromolecular agents for monitoring tumor microvessels and angiogenesis inhibition, Invest. Radiol. 41 (2006) 325–331. https://doi.org/10.1097/01.rli.0000186565.21375.88
[116] S. Santra, D. Dutta, G.A. Walter, B.M. Moudgil, Fluorescent nanoparticle probes for cancer imaging, Technol. Cancer Res. Treat. 4 (2005) 593–602. https://doi.org/10.1177/153303460500400603
[117] K. Kim, J.H. Kim, H. Park, Y.S. Kim, K. Park, H. Nam, S. Lee, J.H. Park, R.W. Park, I.S. Kim, K. Choi, S.Y. Kim, K. Park, I.C. Kwon, Tumor-homing multifunctional nanoparticles for cancer theragnosis: Simultaneous diagnosis, drug delivery, and therapeutic monitoring, J. Control. Release. 146 (2010) 219–227. https://doi.org/10.1016/j.jconrel.2010.04.004
[118] X. Gao, Y. Cui, R.M. Levenson, L.W.K. Chung, S. Nie, In vivo cancer targeting and imaging with semiconductor quantum dots, Nat. Biotechnol. 22 (2004) 969–976. https://doi.org/10.1038/nbt994
[119] X. Cai, W. Li, C.H. Kim, Y. Yuan, L. V. Wang, Y. Xia, In vivo quantitative evaluation of the transport kinetics of gold nanocages in a lymphatic system by noninvasive photoacoustic tomography, ACS Nano. 5 (2011) 9658–9667. https://doi.org/10.1021/nn203124x
[120] A. De La Zerda, C. Zavaleta, S. Keren, S. Vaithilingam, S. Bodapati, Z. Liu, J. Levi, B.R. Smith, T.J. Ma, O. Oralkan, Z. Cheng, X. Chen, H. Dai, B.T. Khuri-Yakub, S.S. Gambhir, Carbon nanotubes as photoacoustic molecular imaging agents in living mice, Nat. Nanotechnol. 3 (2008) 557–562. https://doi.org/10.1038/nnano.2008.231
[121] M.D. Majmudar, J. Yoo, E.J. Keliher, J.J. Truelove, Y. Iwamoto, B. Sena, P. Dutta, A. Borodovsky, K. Fitzgerald, M.F. Di Carli, P. Libby, D.G. Anderson, F.K. Swirski, R. Weissleder, M. Nahrendorf, Polymeric nanoparticle PET/MR imaging allows macrophage detection in atherosclerotic plaques, Circ. Res. 112 (2013) 755–761. https://doi.org/10.1161/CIRCRESAHA.111.300576
[122] H. Xie, Z.J. Wang, A. Bao, B. Goins, W.T. Phillips, In vivo PET imaging and biodistribution of radiolabeled gold nanoshells in rats with tumor xenografts, Int. J. Pharm. 395 (2010) 324–330. https://doi.org/10.1016/j.ijpharm.2010.06.005
[123] O.R. Brouwer, T. Buckle, L. Vermeeren, W.M.C. Klop, A.J.M. Balm, H.G. Van Der Poel, B.W. Van Rhijn, S. Horenblas, O.E. Nieweg, F.W.B. Van Leeuwen, R.A. Valdeś Olmos, Comparing the hybrid fluorescent-radioactive tracer indocyanine green- 99mTc-Nanocolloid with99mTc-nanocolloid for sentinel node identification: A validation study using lymphoscintigraphy and SPECT/CT, J. Nucl. Med. 53 (2012) 1034–1040. https://doi.org/10.2967/jnumed.112.103127
[124] B.E. Ocampo-García, F. de M. Ramírez, G. Ferro-Flores, L.M. De León-Rodríguez, C.L. Santos-Cuevas, E. Morales-Avila, C.A. de Murphy, M. Pedraza-López, L.A. Medina, M.A. Camacho-López, 99mTc-labelled gold nanoparticles capped with HYNIC-peptide/mannose for sentinel lymph node detection, Nucl. Med. Biol. 38 (2011) 1–11. https://doi.org/10.1016/j.nucmedbio.2010.07.007
[125] B. Kumar, R. Kumar, I. Skvortsova, V. Kumar, Mechanisms of Tubulin Binding Ligands to Target Cancer Cells: Updates on their Therapeutic Potential and Clinical Trials, Curr. Cancer Drug Targets. 17 (2017) 357–375. https://doi.org/10.2174/1568009616666160928110818
[126] Y. Xu, K. Jang, T. Yamashita, Y. Tanaka, K. Mawatari, T. Kitamori, Microchip-based cellular biochemical systems for practical applications and fundamental research: from microfluidics to nanofluidics, Anal. Bioanal. Chem. 402 (2011) 99–107. https://doi.org/10.1007/s00216-011-5296-5
[127] A. Ponomaryova, E. Rykova, N. Cherdyntseva, E. Morozkin, I. Zaporozhchenko, T. Skvortsova, A. Dobrodeev, A. Zav’yalov, S. Tuzikov, V. Vlassov, P. Laktionov, P90, Eur. J. Cancer Suppl. 13 (2015) 43–44. https://doi.org/10.1016/j.ejcsup.2015.08.077
[128] X. Chen, R. Park, M. Tohme, A.H. Shahinian, J.R. Bading, P.S. Conti, MicroPET and Autoradiographic Imaging of Breast Cancer αv-Integrin Expression Using 18F- and 64Cu-Labeled RGD Peptide, Bioconjug. Chem. 15 (2003) 41–49. https://doi.org/10.1021/bc0300403
[129] Y.-S. Borghei, M. Hosseini, M.R. Ganjali, Detection of large deletion in human BRCA1 gene in human breast carcinoma MCF-7 cells by using DNA-Silver Nanoclusters, Methods Appl. Fluoresc. 6 (2017) 15001. https://doi.org/10.1088/2050-6120/aa8988
[130] S. Hannenhalli, Faculty Opinions recommendation of Epigenetically reprogrammed methylation landscape drives the DNA self-assembly and serves as a universal cancer biomarker., Fac. Opin. – Post-Publication Peer Rev. Biomed. Lit. (2018). https://doi.org/10.3410/f.734549397.793554291
[131] N. Shehada, G. Brönstrup, K. Funka, S. Christiansen, M. Leja, H. Haick, Ultrasensitive Silicon Nanowire for Real-World Gas Sensing: Noninvasive Diagnosis of Cancer from Breath Volatolome, Nano Lett. 15 (2014) 1288–1295. https://doi.org/10.1021/nl504482t
[132] F.S. Alves, J. de A. Rodrigues Do Rego, M.L. Da Costa, L.F. Lobato Da Silva, R.A. Da Costa, J.N. Cruz, D.D.S.B. Brasil, Spectroscopic methods and in silico analyses using density functional theory to characterize and identify piperine alkaloid crystals isolated from pepper (Piper Nigrum L.), J. Biomol. Struct. Dyn. 38 (2019) 2792–2799. https://doi.org/10.1080/07391102.2019.1639547
[133] Y. Zhu, P. Chandra, Y.-B. Shim, Ultrasensitive and Selective Electrochemical Diagnosis of Breast Cancer Based on a Hydrazine–Au Nanoparticle–Aptamer Bioconjugate, Anal. Chem. 85 (2012) 1058–1064. https://doi.org/10.1021/ac302923k
[134] C.-Y. Wen, L.-L. Wu, Z.-L. Zhang, Y.-L. Liu, S.-Z. Wei, J. Hu, M. Tang, E.-Z. Sun, Y.-P. Gong, J. Yu, D.-W. Pang, Quick-Response Magnetic Nanospheres for Rapid, Efficient Capture and Sensitive Detection of Circulating Tumor Cells, ACS Nano. 8 (2013) 941–949. https://doi.org/10.1021/nn405744f
[135] Y. Liu, Hybrid BaYbF5 Nanoparticles: Novel Binary Contrast Agent for High-Resolution in Vivo X-Ray Computed Tomography Angiography, Springer Theses. (2017) 105–120. https://doi.org/10.1007/978-981-10-6168-4_5
[136] E. Kang, H.S. Min, J. Lee, M.H. Han, H.J. Ahn, I.-C. Yoon, K. Choi, K. Kim, K. Park, I.C. Kwon, Nanobubbles from Gas-Generating Polymeric Nanoparticles: Ultrasound Imaging of Living Subjects, Angew. Chemie Int. Ed. 49 (2009) 524–528. https://doi.org/10.1002/anie.200903841
[137] S. Geninatti Crich, B. Bussolati, L. Tei, C. Grange, G. Esposito, S. Lanzardo, G. Camussi, S. Aime, Magnetic Resonance Visualization of Tumor Angiogenesis by Targeting Neural Cell Adhesion Molecules with the Highly Sensitive Gadolinium-Loaded Apoferritin Probe, Cancer Res. 66 (2006) 9196–9201. https://doi.org/10.1158/0008-5472.can-06-1728
[138] F. Kiessling, B. Morgenstern, C. Zhang, Contrast Agents and Applications to Assess Tumor Angiogenesis In Vivo by Magnetic Resonance Imaging, Curr. Med. Chem. 14 (2007) 77–91. https://doi.org/10.2174/092986707779313516
[139] A. Koukourakis Sofia Koukouraki Michael I., High Intratumoral Accumulation of Stealth Liposomal Doxorubicin in Sarcomas: Rationale for Combination with Radiotherapy, Acta Oncol. (Madr). 39 (2000) 207–211. https://doi.org/10.1080/028418600430789
[140] D. Urbach, M. Lupien, M.R. Karagas, J.H. Moore, Cancer heterogeneity: Origins and implications for genetic association studies, Trends Genet. 28 (2012) 538–543
[141] Y. Liu, N. Zhang, Gadolinium loaded nanoparticles in theranostic magnetic resonance imaging, Biomaterials. 33 (2012) 5363–5375. https://doi.org/10.1016/j.biomaterials.2012.03.084