Ion Exchange Resins for Clinical Applications
Muhammad Hassan Sarfraz, Mohsin Khurshid, Bilal Aslam, Muhammad Asif Zahoor
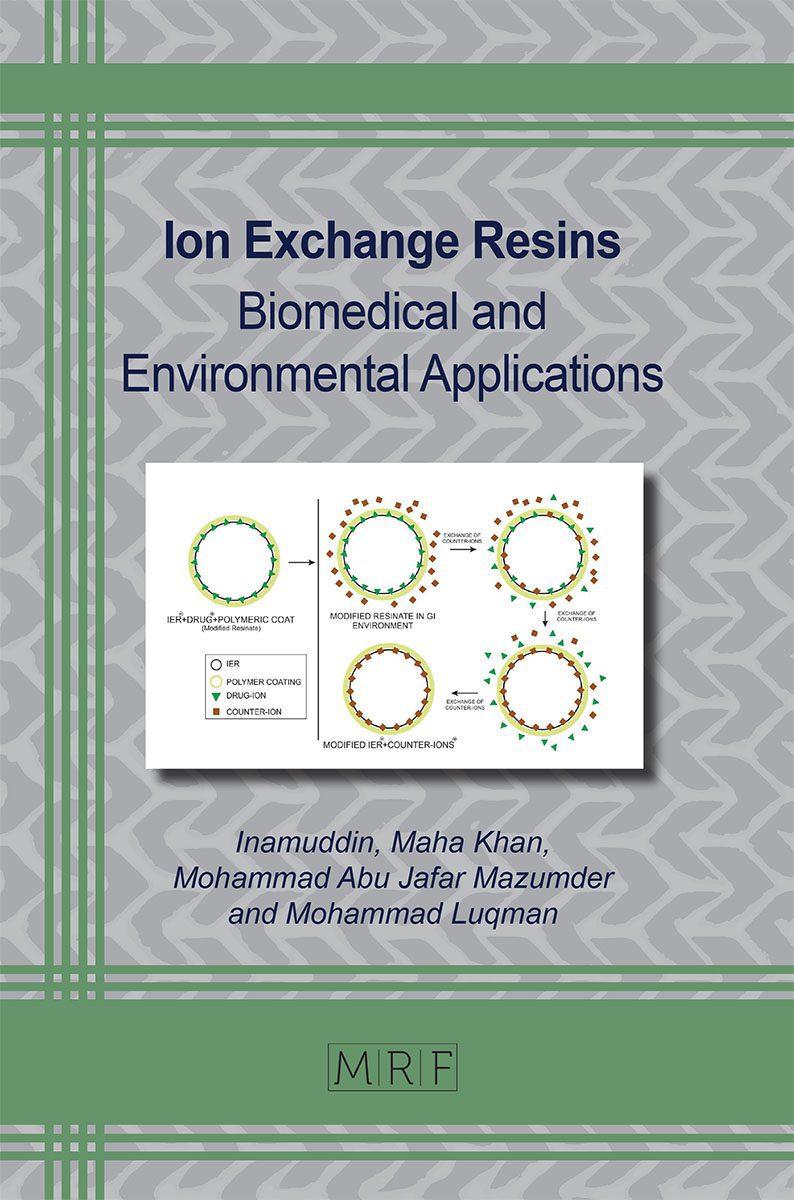
Ion exchange resins are the cross-linked polymers that are insoluble in water and consist of charged ionic groups, for exchanging counter-ions, at repeating positions along the resin. IERs are majorly classified into two types i.e., cationic exchange resins and anionic exchange resins, depending on the type of ion exchanged. Over the last few years, ion exchange resins have gained significant attention owing to their various benefits in drug formulations improving the taste, stability, anti-deliquescence, and dissolution of the drug. They also play a role in targeted drug delivery via employing various delivery technologies such as sigmoidal release system, gastric retentive system, hollow fiber system and microencapsulated resonates. Furthermore, they are also used for therapeutic purposes like treating different ailments and abnormalities such as treating high cholesterol, edema, pruritus, cardiac edema, uremia etc. The chapter presents an overview of the role of ion exchange resins in various clinical implications.
Keywords
Cationic Resins, Anionic Resins, Drug Release, Targeted Drug Delivery, Therapeutics
Published online 12/20/2022, 22 pages
Citation: Muhammad Hassan Sarfraz, Mohsin Khurshid, Bilal Aslam, Muhammad Asif Zahoor, Ion Exchange Resins for Clinical Applications, Materials Research Foundations, Vol. 137, pp 120-141, 2023
DOI: https://doi.org/10.21741/9781644902219-7
Part of the book on Ion Exchange Resins
References
[1] S.D. Alexandratos. Ion-exchange resins: a retrospective from industrial and engineering chemistry research. Industrial & Engineering Chemistry Research, 48(1) (2009) pp.388-398. https://doi.org/10.1021/ie801242v
[2] M.A. Harmer and Q. Sun. Solid acid catalysis using ion-exchange resins. Applied Catalysis A: General, 221(1-2) (2001) 45-62. https://doi.org/10.1016/S0926-860X(01)00794-3
[3] S. Sivaneswari, E. Karthikeyan, D. Veena, P.J. Chandana, P. Subhashree, L. Ramya, R. Rajalakshmi, A.K. CK, Physicochemical characterization of taste masking levetiracetam ion exchange resinates in the solid state and formulation of stable liquid suspension for pediatric use, Beni-Suef Univ. J. Basic Appl. Sci. 5 (2) (2016) 126-133. https://doi.org/10.1016/j.bjbas.2016.04.004
[4] S.H. Jeong, K. Park, Development of sustained release fast-disintegrating tablets using various polymer-coated ion-exchange resin complexes, Int. J. Pharm. 353 (1-2) (2008) 195-204. https://doi.org/10.1016/j.ijpharm.2007.11.033
[5] L. Hughes, Ion exchange resins unique solutions to formulation problems, Pharm. Technol. 22 (2004) 20-25.
[6] S.N. Khan, Therapeutic applications of ion exchange resins, in: Inamuddin, M. Luqman (Eds.), Ion Exchange Technology II, Springer, Dordrech,t 2012, pp. 149-168. https://doi.org/10.1007/978-94-007-4026-6_7
[7] W.P. Arnold Jr., Medical uses of ion-exchange resins, N. Engl. J. Med. 245 (9) (1951) 331-336. https://doi.org/10.1056/NEJM195108302450905
[8] M.A. Hussain, R.C. DiLuccio, E. Shefter, Hollow fibers as an oral sustained-release delivery system, Pharm. Res. 6(1) (1989) 49-52. https://doi.org/10.1023/A:1015847618671
[9] S. Pande, M. Kshirsagar, A. Chandewar, Ion exchange resins pharmaceutical applications and recent advancement, Int. J. Adv. Pharm. 2 (1) (2011).
[10] L.S. Goodman. Goodman and Gilman’s the pharmacological basis of therapeutics, New York: McGraw-Hill. Vol. 1549, (1990) pp. 1361-1373.
[11] N.C. Chaudhry, L. Saunders, Sustained release of drugs from ion exchange resins, J. Pharm. Pharmacol. 8 (1) (1956) 975-986. https://doi.org/10.1111/j.2042-7158.1956.tb12227.x
[12] J.M. Moreau, L.C. Green, L.S. Engel, J.M. Hill, R.J. O’Callaghan, Effectiveness of ciprofloxacin-polystyrene sulfonate (PSS), ciprofloxacin and ofloxacin in a Staphylococcus keratitis model, Curr. Eye Res. 17 (8) (1998) 808-812. https://doi.org/10.1080/02713689808951262
[13] B. Suh, W.A. Craig, A.C. England, R.L. Elliott, Effect of free fatty acids on protein binding of antimicrobial agents, J. Infect. Dis. 143 (4) (1981) 609-616. https://doi.org/10.1093/infdis/143.4.609
[14] D. Shukla, S. Chakraborty, S. Singh and B. Mishra. Mouth dissolving tablets II: An overview of evaluation techniques. Scientia Pharmaceutica, 77(2) (2009) pp.327-342. https://doi.org/10.3797/scipharm.0811-09-02
[15] V. Suhagiya, A. Goyani, R. Gupta, Taste masking by ion exchange resin and its new applications: A review, Int. J. Pharm. Sci. Res. 1 (4) (2010) 22-37.
[16] S. Vijay, C. Dr, Ion exchange resins and their applications, J. Drug Deliv. Ther. 4 (4) (2014) 115-123. https://doi.org/10.22270/jddt.v4i4.925
[17] L. Hughes, New uses of ion exchange resins in pharmaceutical formulation, Pharm. Tech. 17 (2005) 38.
[18] P. Amin, N. Prabhu, and A. Wadhwani. Indion 414 as superdisintegrant in formulation of mouth dissolve tablets. Indian journal of pharmaceutical sciences, 68(1) (2006) p.117. https://doi.org/10.4103/0250-474X.22983
[19] J. Mahore, K. Wadher, M. Umekar, P. Bhoyar, Ion exchange resins: pharmaceutical applications and recent advancement, Int. J. Pharm. Sci. Res. 1 (2) (2010) 8-13.
[20] K. Hänninen, A.M. Kaukonen, T. Kankkunen, J. Hirvonen, Rate and extent of ion-exchange process: the effect of physico-chemical characteristics of salicylate anions, J. Control Release. 91 (3) (2003) 449-463. https://doi.org/10.1016/S0168-3659(03)00276-1
[21] T. Kankkunen, I. Huupponen, K. Lahtinen, M. Sundell, K. Ekman, K. Kontturi, J. Hirvonen, Improved stability and release control of levodopa and metaraminol using ion-exchange fibers and transdermal iontophoresis, Eur. J. Pharm. Sci. 16 (4-5) (2002) 273-280. https://doi.org/10.1016/S0928-0987(02)00113-6
[22] M. Chaubal, Synthetic polymer-based ion exchange resins: excipients & actives, Drug Deliv. Tech. 3 (5) (2003).
[23] A. Bennett, High purity water: Advances in ion exchange technology, Filtr. Sep. 44 (6) (2007) 20-23. https://doi.org/10.1016/S0015-1882(07)70180-5
[24] J.T. Fell, L. Whitehead, J.H. Collett, Prolonged gastric retention: using floating dosage forms, Pharm. Technol. 24 (3) (2000) 82-90.
[25] Y. Chen, M.A. Burton, J.P. Codde, S. Napoli, I.J. Martins, B.N. Gray, Evaluation of Ion‐exchange Microspheres as Carriers for the Anticancer Drug Doxorubicin: In‐vitro Studies, J. Pharm. Pharmacol. 44 (3) (1992) 211-215. https://doi.org/10.1111/j.2042-7158.1992.tb03583.x
[26] S. Burton, N. Washington, R. Steele, R.M. FEELY, Intragastric distribution of ion‐exchange resins: A drug delivery system for the topical treatment of the gastric mucosa, J. Pharm. Pharmacol. 47 (11) (1995) 901-906. https://doi.org/10.1111/j.2042-7158.1995.tb03268.x
[27] F. Atyabi, H. Sharma, H. Mohammad, J. Fell, Controlled drug release from coated floating ion exchange resin beads, J. Control Release. 42 (1) (1996) 25-28. https://doi.org/10.1016/0168-3659(96)01343-0
[28] W. Irwin, R. Machale, P. Watts, Drug-delivery by ion-exchange. Part VII: release of acidic drugs from anionic exchange resinate complexes, Drug Dev. Ind. Pharm. 16 (6) (1990) 883-898. https://doi.org/10.3109/03639049009114916
[29] S. Narisawa, M. Nagata, Y. Hirakawa, M. Kobayashi, H. Yoshino, An organic acid-induced sigmoidal release system for oral controlled-release preparations. III. Elucidation of the anomalous drug release behavior through osmotic pumping mechanism, Int. J. Pharm. 148 (1) (1997) 85-91. https://doi.org/10.1016/S0378-5173(96)04834-X
[30] S. Jackson, D. Bush, A. Perkins, Comparative scintigraphic assessment of the intragastric distribution and residence of cholestyramine, Carbopol 934P and sucralfate, Int. J. Pharm. 212 (1) (2001) 55-62. https://doi.org/10.1016/S0378-5173(00)00600-1
[31] F. Siepmann, J. Siepmann, M. Walther, R. MacRae, R. Bodmeier, Polymer blends for controlled release coatings, J. Control Release. 125 (1) (2008) 1-15. https://doi.org/10.1016/j.jconrel.2007.09.012
[32] M. Kurowski, H. Menninger, E. Pauli, The efficacy and relative bioavailability of diclofenac resinate in rheumatoid arthritis patients, Int. J. Clin. Pharmacol. Ther. 32 (8) (1994) 433-440.
[33] A.U. Kadam, D.M. Sakarkar and P.S. Kawtikwar. Development and evaluation of oral controlled release chlorpheniramine-ion exchange resinate suspension. Indian Journal of Pharmaceutical Sciences, 70(4) (2008) p.531. https://doi.org/10.4103/0250-474X.44613
[34] S. Burton, N. Washington, R. Steele, R.M. FEELY, Intragastric distribution of ion‐exchange resins: A drug delivery system for the topical treatment of the gastric mucosa, J. Pharm. Pharmacol. 47 (11) (1995) 901-906. https://doi.org/10.1111/j.2042-7158.1995.tb03268.x
[35] A. Sawaya, J.P. Benoit, S. Benita, Binding mechanism of doxorubicin in lon‐exchange albumin microcapsules, J. Pharm. Sci. 76 (6) (1987) 475-480. https://doi.org/10.1002/jps.2600760613
[36] R.K. Kamble, C.C. Singh, K.R. Priyadarshani.Current Trends: Ion Exchange Resinates in Controlled Drug Delivery. International Journal of Pharmaceutics and Drug Analysis, 2(1) (2014) 1-11.
[37] V. Anand, R. Kandarapu, S. Garg, Ion-exchange resins: carrying drug delivery forward, Drug Discov. 6 (17) (2001) 905-914. https://doi.org/10.1016/S1359-6446(01)01922-5
[38] I. Singh, A.K. Rehni, R. Kalra, G. Joshi, M. Kumar, H.Y. Aboul-Enein, Ion exchange resins: Drug delivery and therapeutic applications, Fabad J. Pharm. Sci. 32 (2) (2007) 91.
[39] L. Hughes, Ion Exchange Resinates, Pharm. Technol. Eur. 17 (4) (2005) 38-42.
[40] V.B. Junyaprasert, G. Manwiwattanakul, Release profile comparison and stability of diltiazem-resin microcapsules in sustained release suspensions, Int. J. Pharm. 352 (1-2) (2008) 81-91. https://doi.org/10.1016/j.ijpharm.2007.10.018
[41] Y.-H. Cheng, P. Watts, M. Hinchcliffe, R. Hotchkiss, R. Nankervis, N. Faraj, A. Smith, S. Davis, L. Illum, Development of a novel nasal nicotine formulation comprising an optimal pulsatile and sustained plasma nicotine profile for smoking cessation, J. Control Release. 79 (1-3) (2002) 243-254. https://doi.org/10.1016/S0168-3659(01)00553-3
[42] M. Higaki, T. Takase, R. Igarashi, Y. Suzuki, C. Aizawa, Y. Mizushima, Enhancement of immune response to intranasal influenza HA vaccine by microparticle resin, Vaccine. 16 (7) (1998) 741-745. https://doi.org/10.1016/S0264-410X(97)00248-X
[43] L. Yu, S. Li, Y. Yuan, Y. Dai, H. Liu, The delivery of ketoprofen from a system containing ion-exchange fibers, Int. J. Pharm. 319 (1-2) (2006) 107-113. https://doi.org/10.1016/j.ijpharm.2006.03.039
[44] R. Jani, O. Gan, Y. Ali, R. Rodstrom, S. Hancock, Ion exchange resins for ophthalmic delivery, J. Ocul. Pharmacol. Ther. 10 (1) (1994) 57-67. https://doi.org/10.1089/jop.1994.10.57
[45] M.V. Srikanth, S.A. Sunil, N.S. Rao, , M.U. Uhumwangho and K.R. Murthy. Ion-exchange resins as controlled drug delivery carriers. Journal of Scientific Research, 2(3) (2010) pp.597-597. https://doi.org/10.3329/jsr.v2i3.4991
[46] A.J. Hilmer, R.B. Jeffrey, W.G. Park, C. Khosla, Cholestyramine as a promising, strong anion exchange resin for direct capture of genetic biomarkers from raw pancreatic fluids, Biotechnol. Bioeng. 114 (4) (2017) 934-938. https://doi.org/10.1002/bit.26207
[47] T. Suzuki, K. Oba, Y. Igari, N. Matsumura, K. Watanabe, S. Futami-Suda, H. Yasuoka, M. Ouchi, K. Suzuki, Y. Kigawa, Colestimide lowers plasma glucose levels and increases plasma glucagon-like PEPTIDE-1 (7-36) levels in patients with type 2 diabetes mellitus complicated by hypercholesterolemia, J. Nippon. Med. Sch. 74 (5) (2007) 338-343. https://doi.org/10.1272/jnms.74.338
[48] F. Alvarez, Treatments in chronic cholestasis in children, Ann Nestlé [Engl]. 66 (3) (2008) 127-135. https://doi.org/10.1159/000147410
[49] M. Srikanth, S. Sunil, N. Rao, M. Uhumwangho, K.R. Murthy, Ion-exchange resins as controlled drug delivery carriers, J. Sci. Res. 2 (3) (2010) 597-597. https://doi.org/10.3329/jsr.v2i3.4991
[50] D.M. Lichtenwalner, B. Suh, B. Lorber, M.R. Rudnick, W.A. Craig, Correction of drug binding defects in uremia in vitro by anion exchange resin treatment, Biochem. Pharmacol. 31 (21) (1982) 3483-3487. https://doi.org/10.1016/0006-2952(82)90630-X
[51] W.A. Craig, M.A. Evenson, K.P. Sarver, J.P. Wagnild, Correction of protein binding defect in uremic sera by charcoal treatment, J. Lab. Clin. Med. 87 (4) (1976) 637-647.
[52] D. Lichtenwalner, B. Suh, B. Lorber, M. Rudnick, W. Craig, Partial purification and characterization of the drug-binding-defect inducer in uremia, J. Lab. Clin. Med. 97 (1) (1981) 72-81.