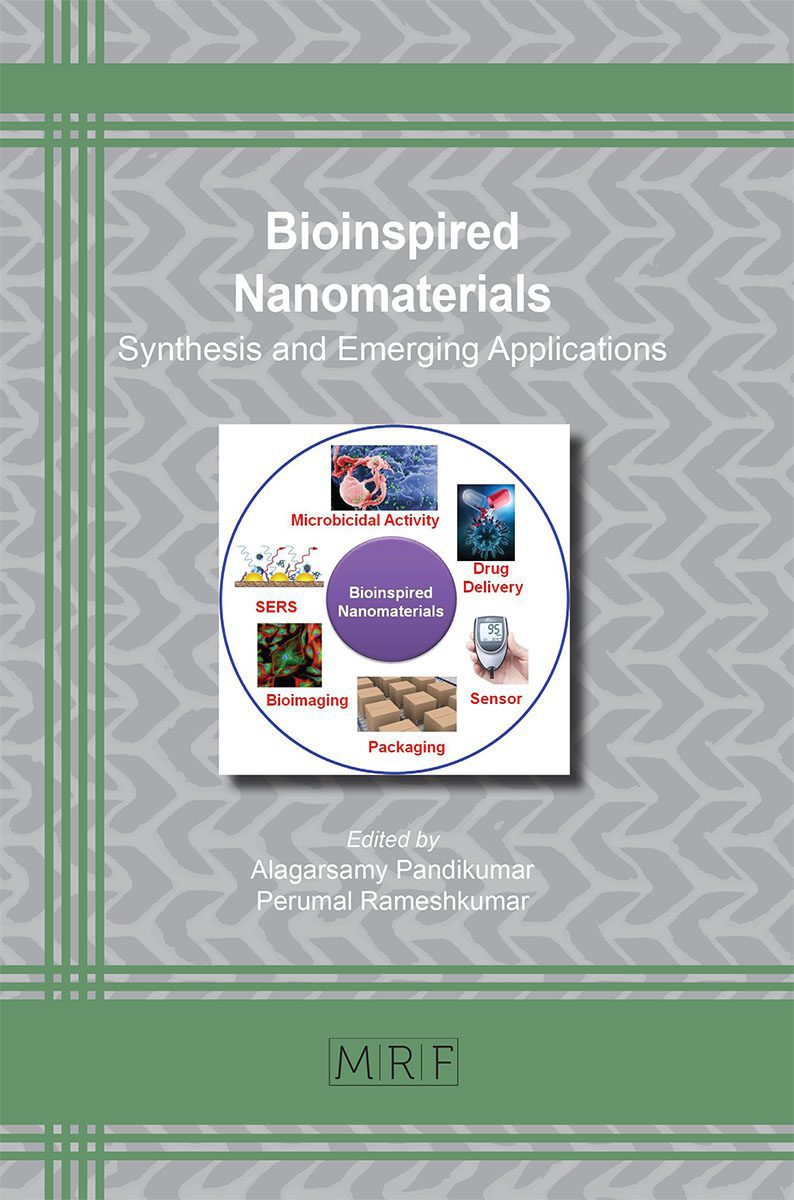
Bioinspired Nanomaterials for Drug Delivery
Balaji Maddiboyina, Jeyabalan Shanmugapriya, Swetha Rasala, Gandhi Sivaraman
Over the preceding few decades therapeutic/drug delivery systems were explored and investigated as a tactic to advance the efficiency and safety of therapeutic agents for various biomedical applications. Nano-engineering on the various biomaterials are reported and are under investigation to enhance the pharmacokinetics and pharmacodynamics of many drugs, with proven enhancements in terms of objective facility, therapeutic efficacy, reduction in dosing frequency and associated drug side effects. Bioinspired materials from various sources (biomass, plants, animals, cells, biotechnology interventions) are of great interest with additive advantages over synthetic materials in terms of biocompatibility, biodegradation, nontoxicity, non-immunogenic and are cost effective systems. Bioinspired nano platforms are proceeding round the world to contrive novel drug delivery carriers using different strategies. This chapter encompasses encroachments in the diverse types of bioinspired polymers and their nano delivery systems. Comprehensive evidence is also concise on delivery systems morphological, biological functionalities from respectively material and their potentialities as persuasive carriers for drug delivery systems.
Keywords
Nanomaterials, Nanodelivery Systems, Nanoparticles, Nanotherapies
Published online 8/10/2021, 33 pages
Citation: Balaji Maddiboyina, Jeyabalan Shanmugapriya, Swetha Rasala, Gandhi Sivaraman, Bioinspired Nanomaterials for Drug Delivery, Materials Research Foundations, Vol. 111, pp 63-95, 2021
DOI: https://doi.org/10.21741/9781644901571-3
Part of the book on Bioinspired Nanomaterials
References
[1] Aricò AS, Bruce P, Scrosati B, Tarascon J-M, Van Schalkwijk W. 2005. Nanostructured materials for advanced energy conversion and storage devices. Nat. Mater. 4, 366-377. https://doi.org/10.1038/nmat1368
[2] Du D, Yang Y, Lin Y. 2012. Graphene-based materials for biosensing and bioimaging. MRS Bull. 37, 1290-1296. https://doi.org/10.1557/mrs.2012.209
[3] Gaharwar AK, Peppas NA, Khademhosseini A. Biotechnol. Bioeng. 2014, 111, 441-453. https://doi.org/10.1002/bit.25160
[4] Walcarius A, Minteer SD, Wang J, Lin Y, Merkoci A. 2013. Nanomaterials for bio-functionalized electrodes: recent trends. J. Mater. Chem. B 1, 4878-4908. https://doi.org/10.1039/c3tb20881h
[5] Zhou H, Fan T, Zhang D. 2011. Biotemplated materials for sustainable energy and environment: current status and challenges. ChemSusChem 4, 1344-1387. https://doi.org/10.1002/cssc.201100048
[6] An FF, Zhang XH. Strategies for Preparing Albumin-based Nanoparticles for Multifunctional Bioimaging and Drug Delivery. Theranostics. 2017;7(15):3667‐3689. https://doi.org/10.7150/thno.19365
[7] Sotiropoulou S, Sierra-Sastre Y, Mark SS, Batt CA. 2008. Biotemplated nanostructured materials. Chem. Mater. 20, 821-834. https://doi.org/10.1021/cm702152a
[8] Zhao M, Lei C, Yang Y, et al. Abraxane, the Nanoparticle Formulation of Paclitaxel Can Induce Drug Resistance by Up-Regulation of P-gp. PLoS One. 2015;10(7):e0131429. https://doi.org/10.1371/journal.pone.0131429
[9] Saravanakumar G, Jo DG, Park JH. Polysaccharide-based nanoparticles: a versatile platform for drug delivery and biomedical imaging. Curr Med Chem. 2012;19(19):3212‐3229. https://doi.org/10.2174/092986712800784658
[10] Swierczewska M, Han HS, Kim K, Park JH, Lee S. Polysaccharide-based nanoparticles for theranostic nanomedicine. Adv Drug Deliv Rev. 2016; 99(Pt A):70‐84. https://doi.org/10.1016/j.addr.2015.11.015
[11] Huh MS, Lee EJ, Koo H, et al. Polysaccharide-based Nanoparticles for Gene Delivery. Top Curr Chem (Cham). 2017;375(2):31. https://doi.org/10.1007/s41061-017-0114-y
[12] Hudak JE, Bertozzi CR. Glycotherapy: new advances inspire a reemergence of glycans in medicine. Chem Biol. 2014;21(1):16‐37. https://doi.org/10.1016/j.chembiol.2013.09.010
[13] Agard NJ, Bertozzi CR. Chemical approaches to perturb, profile, and perceive glycans. Acc. Chem. Res. 2009;42:788-797. https://doi.org/10.1021/ar800267j
[14] Arnold JN, Wormald MR, Sim RB, Rudd PM, Dwek RA. The impact of glycosylation on the biological function and structure of human immunoglobulins. Annu. Rev. Immunol. 2007;25:21-50. https://doi.org/10.1146/annurev.immunol.25.022106.141702
[15] Trombino S, Servidio C, Curcio F, Cassano R. Strategies for Hyaluronic Acid-Based Hydrogel Design in Drug Delivery. Pharmaceutics. 2019;11(8):407. https://doi.org/10.3390/pharmaceutics11080407
[16] G.R.M. Jillian, M.E. Van Dyke, A review of keratin-based biomaterials for biomedical applications, Dent. Mater. 3 (2010) 999-1014. https://doi.org/10.3390/ma3020999
[17] Brandelli A. Bacterial keratinases: useful enzymes for bioprocessing agroindustrial wastes and beyond, Food Bioproc. Tech. 1 (2) (2008) 105-116. https://doi.org/10.1007/s11947-007-0025-y
[18] M.A. Khosa, A. Ullah, A sustainable role of keratin biopolymer in green chemistry: a review, J. Food Process. Beverag. 1 (1) (2013) 8.
[19] L. Kreplak, J. Doucet, P. Dumas, F. Briki, New aspects of the α-helix to β-sheet transition in stretched hard α-keratin fibers, Biophys. J. 87 (1) (2004) 640-647. https://doi.org/10.1529/biophysj.103.036749
[20] A. Aluigi, C. Tonetti, C. Vineis, C. Tonin, G. Mazzuchetti, Adsorption of copper (II) ions by keratin/PA6 blend nanofibres, Eur. Polym. J. 47 (9) (2011) 1756-1764. https://doi.org/10.1016/j.eurpolymj.2011.06.009
[21] A. Ghosh, S.R. Collie, Keratinous materials as novel absorbent systems for toxic Pollutants, Def. Sci. J. 64 (3) (2014) 209-221. https://doi.org/10.14429/dsj.64.7319
[22] Verma, V.; Verma, P.; Ray, P.; Ray, A.R. Preparation of scaffolds from human hair proteins for tissue-engineering applications. Biomed. Mater. 2008, 3, 25007. https://doi.org/10.1088/1748-6041/3/2/025007
[23] Dai L, Si C. Recent Advances on Cellulose-Based Nano-Drug Delivery Systems: Design of Prodrugs and Nanoparticles. Curr Med Chem. 2019; 26(14):2410‐2429. https://doi.org/10.2174/0929867324666170711131353
[24] Esposito A, Sannino A, Cozzolino A, Nappo QS, Lamberti M, Ambrosio L, Nicolais L (2005) Response of intestinal cells and macrophages to an orally administered cellulose-PEG based polymer as a potential treatment for intractable edemas. Biomaterials 26:4101-4110 https://doi.org/10.1016/j.biomaterials.2004.10.023
[25] Sezer S., Şahin İ., Öztürk K., Şanko V., Koçer Z., Sezer Ü.A. (2019) Cellulose-Based Superabsorbent Hydrogels. Polymers and Polymeric Composites: Cellulose-Based Superabsorbent Hydrogels. 1177-1203. https://doi.org/10.1007/978-3-319-77830-3_40
[26] L. Bedian, A.M.V. Rodríguez, G.H. Vargas, R. Parra-Saldivar, H.M.N. Iqbal, Bio-based materials with novel characteristics for tissue engineering applications-a review, Int. J. Biol. Macromol. 98 (2017) 837-846. https://doi.org/10.1016/j.ijbiomac.2017.02.048
[27] N. Singh, J. Chen, K.K. Koziol, K.R. Hallam, D. Janas, A.J. Patil. Chitin and carbon nanotube composites as biocompatible scaffolds for neuron growth, Nanoscale. 8 (15); 2016: 8288-8299. https://doi.org/10.1039/C5NR06595J
[28] S. Cammas, M.-M. Béar, L. Moine et al., “Polymers of malic acid and 3-alkylmalic acid as synthetic PHAs in the design of biocompatible hydrolyzable devices,” International Journal of Biological Macromolecules. 1999; 25: 273-282. https://doi.org/10.1016/S0141-8130(99)00042-2
[29] G.-Q. Chen, “A microbial polyhydroxyalkanoates (PHA) based bio- and materials industry,” Chemical Society Reviews. 2009; 38(8): 2434-2446. https://doi.org/10.1039/b812677c
[30] R. Acharya, S. Saha, S. Ray, S. Hazra, M.K. Mitra, J. Chakraborty. siRNA-nanoparticle conjugate in gene silencing: a future cure to deadly diseases? Mater. Sci. Eng. C Mater. Biol. Appl., 76 (2017), 1378-1400. https://doi.org/10.1016/j.msec.2017.03.009
[31] Caitriona M.O’D, Andreas BS, Julian DF, Véronique P, Vincent J. Oral delivery of non-viral nucleic acid-based therapeutics – do we have the guts for this? European Journal of Pharmaceutical Sciences. 2019; 133: 190-204. https://doi.org/10.1016/j.ejps.2019.03.027
[32] Weng T, Qi J, Lu Y, et al. The role of lipid-based nano delivery systems on oral bioavailability enhancement of fenofibrate, a BCS II drug: comparison with fast-release formulations. J Nanobiotechnology. 2014;12:39. https://doi.org/10.1186/s12951-014-0039-3
[33] Hua S. Lipid-based nano-delivery systems for skin delivery of drugs and bioactives. Front Pharmacol. 2015; 6: 219. https://doi.org/10.3389/fphar.2015.00219
[34] Sonaje K, Lin KJ, Tseng MT, Wey SP, Su FY, Chuang EY, Hsu CW, Chen CT, Sung HW. Effects of chitosan-nanoparticle-mediated tight junction opening on the oral absorption of endotoxins. Biomaterials. 2011;32:8712-8721. https://doi.org/10.1016/j.biomaterials.2011.07.086
[35] Beuttler J, Rothdiener M, Muller D, Frejd FY, Kontermann RE. Targeting of epidermal growth factor receptor (EGFR)-expressing tumor cells with sterically stabilized affibody liposomes (SAL) Bioconjug Chem. 2009;20(6):1201-1208. https://doi.org/10.1021/bc900061v
[36] Wissing SA, Muller RH. The influence of solid lipid nanoparticles on skin hydration and viscoelasticity – in vivo study. Eur J Pharm Biopharm. 2003; 56(1): 67-72. https://doi.org/10.1016/S0939-6411(03)00040-7
[37] Schubert MA, Muller-Goymann CC. Characterisation of surface-modified solid lipid nanoparticles (SLN). Influence of lecithin and nonionic emulsifier. Eur J Pharm Biopharm. 2005;61(1-2):77-86. https://doi.org/10.1016/j.ejpb.2005.03.006
[38] Muller RH, Radtke M, Wissing SA. Nanostructured lipid matrices for improved microencapsulation of drugs. Int J Pharm. 2002;242(1-2):121-128. https://doi.org/10.1016/S0378-5173(02)00180-1
[39] Teeranachaideekul V, Muller RH, Junyaprasert VB. Encapsulation of ascorbyl palmitate in nanostructured lipid carriers (NLC) – Effects of formulation parameters on physicochemical stability. Int J Pharm. 2007; 340(1-2):198-206. https://doi.org/10.1016/j.ijpharm.2007.03.022
[40] Sunderland K.S., Yang M., Mao C. Phage-Enabled Nanomedicine: From Probes to Therapeutics in Precision Medicine. Angew. Chem. 2017; 56:1964-1992. https://doi.org/10.1002/anie.201606181
[41] Banwell EF, Abelardo ES, Adams DJ, et al. Rational design and application of responsive alpha-helical peptide hydrogels. Nat Mater. 2009; 8(7): 596‐600. https://doi.org/10.1038/nmat2479
[42] Sokullu E, Soleymani Abyaneh H, Gauthier MA. Plant/Bacterial Virus-Based Drug Discovery, Drug Delivery, and Therapeutics. Pharmaceutics. 2019; 11(5):211. https://doi.org/10.3390/pharmaceutics11050211
[43] Koutsopoulos S. Self-assembling peptide nanofiber hydrogels in tissue engineering and regenerative medicine: Progress, design guidelines, and applications. J Biomed Mater Res A. 2016; 104(4):1002‐1016. https://doi.org/10.1002/jbm.a.35638
[44] Aggeli A., Bell M., Carrick L.M., Fishwick C.W.G., Harding R., Mawer P.J., Radford S.E., Strong A.E., Boden N. pH as a trigger of peptide β-sheet self-assembly and reversible switching between nematic and isotropic phases. J. Am. Chem. Soc. 2003;125:9619-9628. https://doi.org/10.1021/ja021047i
[45] Van Hell AJ, Costa CICA, Flesch FM, Sutter M, Jiskoot W, Crommelin DJA, Hennink WE, Mastrobattista E. Self-Assembly of Recombinant Amphiphilic Oligopeptides into Vesicles. Biomacromolecules. 2007; 8: 2753-2761. https://doi.org/10.1021/bm0704267
[46] Thomas CE, Ehrhardt A, Kay M. Progress and Problems with the Use of Viral Vectors for Gene Therapy. Nat Rev Genet. 2003;4:346-358. https://doi.org/10.1038/nrg1066
[47] Garg, H., Mehmetoglu-Gurbuz, T. & Joshi, A. Virus Like Particles (VLP) as multivalent vaccine candidate against Chikungunya, Japanese Encephalitis, Yellow Fever and Zika Virus. Sci Rep 10, 4017 (2020). https://doi.org/10.1038/s41598-020-61103-1
[48] Kaneda Y. Virosomes: evolution of the liposome as a targeted drug delivery system. Adv Drug Deliv Rev. 2000;43(2-3):197‐205. https://doi.org/10.1016/S0169-409X(00)00069-7
[49] Somiya M, Liu Q, Kuroda S. Current Progress of Virus-mimicking Nanocarriers for Drug Delivery. Nanotheranostics. 2017;1(4):415‐429. https://doi.org/10.7150/ntno.21723
[50] Bungener L, Serre K, Bijl L. et al. Virosome-Mediated Delivery of Protein Antigens to Dendritic Cells. Vaccine. 2002;20:2287-2295 https://doi.org/10.1016/S0264-410X(02)00103-2
[51] Tan S, Wu T, Zhang D, Zhang Z. Cell or cell membrane-based drug delivery systems. Theranostics. 2015;5(8):863‐881. https://doi.org/10.7150/thno.11852
[52] Patel PD, Dand N, Hirlekar RS, Kadam VJ. Drug loaded erythrocytes: as novel drug delivery system. Curr Pharm Des. 2008;14(1):63‐70. https://doi.org/10.2174/138161208783330772
[53] Aryal S, Hu CM, Fang RH, et al. Erythrocyte membrane-cloaked polymeric nanoparticles for controlled drug loading and release. Nanomedicine (Lond). 2013;8(8):1271‐1280. https://doi.org/10.2217/nnm.12.153
[54] Lim S, Park J, Shim MK, et al. Recent advances and challenges of repurposing nanoparticle-based drug delivery systems to enhance cancer immunotherapy. Theranostics. 2019;9(25):7906‐7923. https://doi.org/10.7150/thno.38425
[55] Liu X, Li Y, Sun X, Muftuoglu Y, Wang B, Yu T. et al. Powerful anti-colon cancer effect of modified nanoparticle-mediated IL-15 immunogene therapy through activation of the host immune system. Theranostics. 2018;8:3490-503. https://doi.org/10.7150/thno.24157
[56] Orive G, Cobos R, Gorriti J, Pedraz JL, Meregalli M, Torrente Y. Drug delivery technologies and stem cells for tissue repair and regeneration. Curr Pharm Biotechnol. 2015;16(7):646‐654. https://doi.org/10.2174/138920101607150427112457
[57] Shi Q, Montgomery RR. Platelets as delivery systems for disease treatments. Adv Drug Deliv Rev. 2010;62(12):1196‐1203. https://doi.org/10.1016/j.addr.2010.06.007