Polysaccharide Membranes for Drug Delivery System in the Skin Lesion
L.N. Andrade, D.M.L. Oliveira, C.F. Silva, R.G. Amaral, M.V. Chaud, E. Souto, Su Shin Ryon, P. Severino
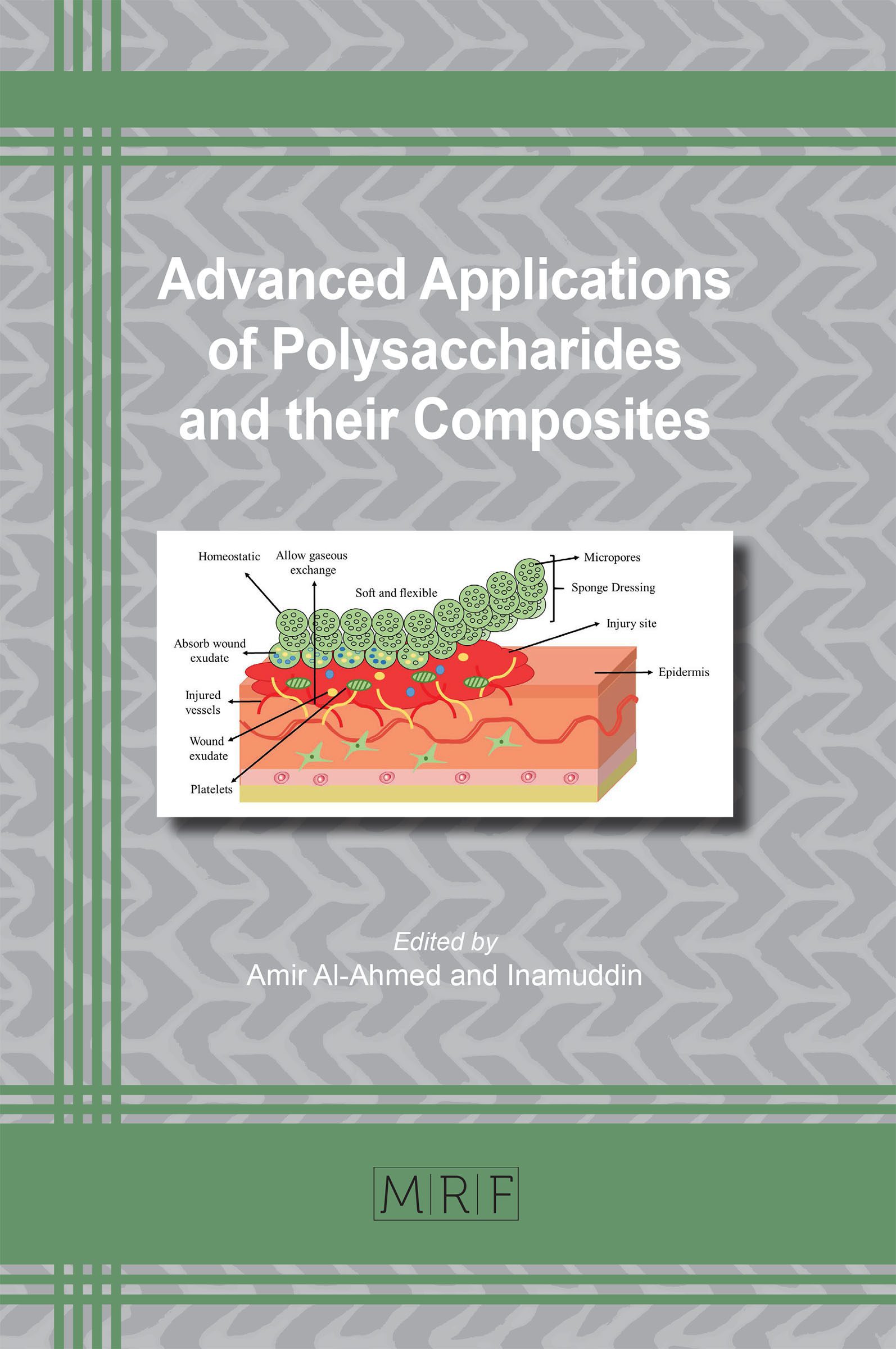
This chapter described the importance of polysaccharides-based membranes for drug delivery systems. The most recent advances in the treatment of skin lesions are related to the use of biomaterials with biological activity that contribute to the cicatrization, reducing the time of cure of the renovated tissue. Polysaccharides are the structural material used in the development of these new dressings because it is biocompatibility and biodegradability. Also, the incorporation of the drug in membrane drug delivery showed to be efficient for treatment. However, the search for an ideal dressing is still underway.
Keywords
Membrane, Wound Healing, Polysaccharide, Drug Delivery, Drug
Published online 4/20/2020, 21 pages
Citation: L.N. Andrade, D.M.L. Oliveira, C.F. Silva, R.G. Amaral, M.V. Chaud, E. Souto, Su Shin Ryon, P. Severino, Polysaccharide Membranes for Drug Delivery System in the Skin Lesion, Materials Research Foundations, Vol. 73, pp 65-85, 2020
DOI: https://doi.org/10.21741/9781644900772-3
Part of the book on Advanced Applications of Polysaccharides and their Composites
References
[1] H. Sorg, D.J. Tilkorn, S. Hager, J. Hauser, U.J. Mirastschijski, Skin wound healing: an update on the current knowledge and concepts, Eur. Surg. Res. 58 (2017) 81-94. https://doi.org/10.1159/000454919
[2] Z.D. Draelos, Skin lightening preparations and the hydroquinone controversy, Dermatol. Ther. 20 (2007) 308-313. https://doi.org/10.1111/j.1529-8019.2007.00144.x
[3] B. Horst, G. Chouhan, N.S. Moiemen, L.M, Advances in keratinocyte delivery in burn wound care, Adv. Drug Deliv. Rev. 123 (2018) 18-32. https://doi.org/10.1016/j.addr.2017.06.012
[4] K. Järbrink, G. Ni, H. Sönnergren, A. Schmidtchen, C. Pang, R. Bajpai, J.J., Prevalence and incidence of chronic wounds and related complications: a protocol for a systematic review, Syst. Rev. 5 (2016) 152. https://doi.org/10.1186/s13643-016-0329-y
[5] I. Garcia-Orue, G. Gainza, F.B. Gutierrez, J.J. Aguirre, C. Evora, J.L. Pedraz, R.M. Hernandez, A. Delgado, M. Igartua, Novel nanofibrous dressings containing rhEGF and Aloe vera for wound healing applications, Int. J. Pharm. 523 (2017) 556-566. https://doi.org/10.1016/j.ijpharm.2016.11.006
[6] R. Capoano, R. Businaro, B. Kolce, A. Biancucci, S. Izzo, L. De Felice, B. Salvati, Multidisciplinary Approaches to the Stimulation of Wound Healing and Use of Dermal Substitutes in Chronic Phlebostatic Ulcers, Wound Healing-Current Perspectives, IntechOpen2019. https://doi.org/10.5772/intechopen.81791
[7] M. Schrementi, L. Chen, L.A. DiPietro, The importance of targeting inflammation in skin regeneration, Skin Tissue Models, Elsevier 2018, pp. 255-275. https://doi.org/10.1016/B978-0-12-810545-0.00011-5
[8] J. Davidson, Current concepts in wound management and wound healing products, Vet Clin North Am Small Anim. Pract. 45 (2015) 537-564. https://doi.org/10.1016/j.cvsm.2015.01.009
[9] H.S. Debone, P.S. Lopes, P. Severino, C.M.P. Yoshida, E.B. Souto, C.F. da Silva, Chitosan/Copaiba oleoresin films for would dressing application, Int. J. Pharm. 555 (2019) 146-152. https://doi.org/10.1016/j.ijpharm.2018.11.054
[10] P.B. Milan, S. Kargozar, M.T. Joghataie, A. Samadikuchaksaraei, Nanoengineered biomaterials for skin regeneration, Nanoengineered Biomaterials for Regenerative Medicine, Elsevier 2019, pp. 265-283. https://doi.org/10.1016/B978-0-12-813355-2.00011-9
[11] M. Naseri-Nosar, Z.M.J.C.p. Ziora, Wound dressings from naturally-occurring polymers: A review on homopolysaccharide-based composites, Carbohydr. Polym. 189 (2018) 379-398. https://doi.org/10.1016/j.carbpol.2018.02.003
[12] A. Sandak, J. Sandak, M. Brzezicki, A. Kutnar, Biomaterials for Building Skins, Bio-based Building Skin, Springer 2019, pp. 27-64. https://doi.org/10.1007/978-981-13-3747-5_2
[13] M. Niinomi, Design and development of metallic biomaterials with biological and mechanical biocompatibility, J. Biomed. Mater. Res. A. 107 (2019) 944-954. https://doi.org/10.1002/jbm.a.36667
[14] D. Rodrigues, A.C. Viotto, R. Checchia, A. Gomide, D. Severino, R. Itri, M.S. Baptista, W.K. Martins, Mechanism of Aloe Vera extract protection against UVA: shelter of lysosomal membrane avoids photodamage, Photochem. Photobiol. Sci. 15 (2016) 334-350. https://doi.org/10.1039/C5PP00409H
[15] P. Severino, A. Feitosa, I. Lima-Verde, M. Chaud, C. Da Silva, R. De Lima, R. Amaral, L. Andrade, Production and Characterization of Mucoadhesive Membranes for Anesthetic Vehiculation, Chem. Eng. Transactions. 64 (2018) 421-426.
[16] P. Balakrishnan, V. Geethamma, M.S. Sreekala, S. Thomas, Polymeric biomaterials: State-of-the-art and new challenges, Fundamental Biomaterials: Polymers, Elsevier 2018, pp. 1-20. https://doi.org/10.1016/B978-0-08-102194-1.00001-3
[17] J.H. Shepherd, D. Howard, A.K. Waller, H.R. Foster, A. Mueller, T. Moreau, A.L. Evans, M. Arumugam, G.B. Chalon, E.J.B. Vriend, Structurally graduated collagen scaffolds applied to the ex vivo generation of platelets from human pluripotent stem cell-derived megakaryocytes: Enhancing production and purity, J. Biomaterials. 182 (2018) 135-144. https://doi.org/10.1016/j.biomaterials.2018.08.019
[18] N. Kamaly, B. Yameen, J. Wu, O. Farokhzad, Degradable controlled-release polymers and polymeric nanoparticles: mechanisms of controlling drug release, Chem. Rev. 116 (2016) 2602-2663. https://doi.org/10.1021/acs.chemrev.5b00346
[19] T.A. Saleh, V.K. Gupta, Nanomaterial And Polymer Membranes: Synthesis, Characterization, And Applications, Elsevier 2016.
[20] H. Hamedi, S. Moradi, S.M. Hudson, A. Tonelli, Chitosan based hydrogels and their applications for drug delivery in wound dressings: A review, Carbohydr. Polym. 199 (2018) 445-460. https://doi.org/10.1016/j.carbpol.2018.06.114
[21] B. Joseph, R. Augustine, N. Kalarikkal, S. Thomas, B. Seantier, Y. Grohens, Recent advances in electrospun polycaprolactone based scaffolds for wound healing and skin bioengineering applications, Mater Today Commun. 19 (2019) 319-335. https://doi.org/10.1016/j.mtcomm.2019.02.009
[22] P.B. Albuquerque, P.A. Soares, A.C. Aragão-Neto, G.S. Albuquerque, L.C. Silva, M.H. Lima-Ribeiro, J.C.S. Neto, L.C. Coelho, M.T. Correia, J.A. Teixeira, Healing activity evaluation of the galactomannan film obtained from Cassia grandis seeds with immobilized Cratylia mollis seed lectin, Int. J. Biol. Macromol. 102 (2017) 749-757. https://doi.org/10.1016/j.ijbiomac.2017.04.064
[23] N. Ninan, A. Forget, V.P. Shastri, N.H. Voelcker, A. Blencowe, Antibacterial and anti-inflammatory pH-responsive tannic acid-carboxylated agarose composite hydrogels for wound healing, ACS Appl. Mater. Interfaces. 8 (2016) 28511-28521. https://doi.org/10.1021/acsami.6b10491
[24] S.P. Miguel, M.P. Ribeiro, H. Brancal, P. Coutinho, I. Correia, Thermoresponsive chitosan–agarose hydrogel for skin regeneration, Carbohydr. Polym. 111 (2014) 366-373. https://doi.org/10.1016/j.carbpol.2014.04.093
[25] W.S. Tan, P. Arulselvan, S.-F. Ng, C.N.M. Taib, M.N. Sarian, S. Fakurazi, Improvement of diabetic wound healing by topical application of Vicenin-2 hydrocolloid film on Sprague Dawley rats, BMC Complement Altern. Med. 19 (2019) 20. https://doi.org/10.1186/s12906-018-2427-y
[26] I. Rubio-Elizalde, J. Bernáldez-Sarabia, A. Moreno-Ulloa, C. Vilanova, P. Juárez, A. Licea-Navarro, A. Castro-Ceseña, Scaffolds based on alginate-PEG methyl ether methacrylate-Moringa oleifera-Aloe vera for wound healing applications, Carbohydr. Polym. 206 (2019) 455-467. https://doi.org/10.1016/j.carbpol.2018.11.027
[27] T. Wang, Y. Zheng, Y. Shi, L. Zhao, pH-responsive calcium alginate hydrogel laden with protamine nanoparticles and hyaluronan oligosaccharide promotes diabetic wound healing by enhancing angiogenesis and antibacterial activity, Drug. Deliv. Transl. Res. 9 (2019) 227-239. https://doi.org/10.1007/s13346-018-00609-8
[28] A. Montaser, M. Rehan, M.E. El-Naggar, pH-Thermosensitive hydrogel based on polyvinyl alcohol/sodium alginate/N-isopropyl acrylamide composite for treating re-infected wounds, Int. J. Biol. Macromol. 124 (2019) 1016-1024. https://doi.org/10.1016/j.ijbiomac.2018.11.252
[29] H. Türe, Characterization of hydroxyapatite-containing alginate–gelatin composite films as a potential wound dressing, Int. J. Biol. Macromol. 123 (2019) 878-888. https://doi.org/10.1016/j.ijbiomac.2018.11.143
[30] M.A.G. Barbosa, A.O. Paggiaro, V.F. de Carvalho, C. Isaac, R. Gemperli, Effects of hydrogel with enriched sodium alginate in wounds of diabetic patients, Plast. Surg. Nurs. 38 (2018) 133-138. https://doi.org/10.1097/PSN.0000000000000228
[31] A. Ahmed, J. Boateng, Calcium alginate-based antimicrobial film dressings for potential healing of infected foot ulcers, Ther. Deliv. 9 (2018) 185-204. https://doi.org/10.4155/tde-2017-0104
[32] M. Summa, D. Russo, I. Penna, N. Margaroli, I.S. Bayer, T. Bandiera, A. Athanassiou, R. Bertorelli, A biocompatible sodium alginate/povidone iodine film enhances wound healing, Eur. J. Pharm. Biopharm. 122 (2018) 17-24. https://doi.org/10.1016/j.ejpb.2017.10.004
[33] M. Li, H. Li, X. Li, H. Zhu, Z. Xu, L. Liu, J. Ma, M. Zhang, A bioinspired alginate-gum arabic hydrogel with micro-/nanoscale structures for controlled drug release in chronic wound healing, ACS Appl. Mater. Interfaces. 9 (2017) 22160-22175. https://doi.org/10.1021/acsami.7b04428
[34] S. Dhall, J.P. Silva, Y. Liu, M. Hrynyk, M. Garcia, A. Chan, J. Lyubovitsky, R.J. Neufeld, M. Martins-Green, Release of insulin from PLGA–alginate dressing stimulates regenerative healing of burn wounds in rats, Clin. Sci. (Lond). 129 (2015) 1115-1129. https://doi.org/10.1042/CS20150393
[35] S. Rossi, M. Mori, B. Vigani, M. Bonferoni, G. Sandri, F. Riva, C. Caramella, F. Ferrari, A novel dressing for the combined delivery of platelet lysate and vancomycin hydrochloride to chronic skin ulcers: Hyaluronic acid particles in alginate matrices, Eur. J. Pharm. Sci. 118 (2018) 87-95. https://doi.org/10.1016/j.ejps.2018.03.024
[36] M. Rezvanian, M.C.I.M. Amin, S.-F. Ng, Development and physicochemical characterization of alginate composite film loaded with simvastatin as a potential wound dressing, Carbohydr. Polym. 137 (2016) 295-304. https://doi.org/10.1016/j.carbpol.2015.10.091
[37] J.S. Boateng, H.V. Pawar, J. Tetteh, Polyox and carrageenan based composite film dressing containing anti-microbial and anti-inflammatory drugs for effective wound healing,Int. J. Pharm. 441 (2013) 181-191. https://doi.org/10.1016/j.ijpharm.2012.11.045
[38] W. Sajjad, T. Khan, M. Ul-Islam, R. Khan, Z. Hussain, A. Khalid, F. Wahid, Development of modified montmorillonite-bacterial cellulose nanocomposites as a novel substitute for burn skin and tissue regeneration, Carbohydr. Polym. 206 (2019) 548-556. https://doi.org/10.1016/j.carbpol.2018.11.023
[39] J.J. Park, J.E. Kim, W.B. Yun, M.R. Lee, J.Y. Choi, B.R. Song, H.J. Son, Y. Lim, H.G. Kang, B.S. An, Therapeutic effects of a liquid bandage prepared with cellulose powders from Styelaáclava tunics and Broussonetiaákazinoki bark: Healing of surgical wounds on the skin of Sprague Dawley rats, Mol. Med. Rep. 19 (2019) 452-460. https://doi.org/10.3892/mmr.2018.9668
[40] T. Maver, L. Gradišnik, D.M. Smrke, K.S. Kleinschek, U. Maver, Systematic evaluation of a diclofenac-loaded carboxymethyl cellulose-based wound dressing and its release performance with changing ph and temperature, AAPS Pharm Sci. Tech. 20 (2019) 29. https://doi.org/10.1208/s12249-018-1236-4
[41] S. Napavichayanun, S. Ampawong, T. Harnsilpong, A. Angspatt, P. Aramwit, Inflammatory reaction, clinical efficacy, and safety of bacterial cellulose wound dressing containing silk sericin and polyhexamethylene biguanide for wound treatment, Arch. Dermatol. Res. 310 (2018) 795-805. https://doi.org/10.1007/s00403-018-1871-3
[42] M.D. Umebayashi Zanoti, H. Megumi Sonobe, S.J. Lima Ribeiro, A.M. Minarelli Gaspar, Development of coverage and its evaluation in the treatment of chronic wounds, Invest. Educ. Enferm. 35 (2017) 330-339. https://doi.org/10.17533/udea.iee.v35n3a09
[43] K. Cutting, The cost-effectiveness of a novel soluble beta-glucan gel, J. Wound Care. 26 (2017) 228-234. https://doi.org/10.12968/jowc.2017.26.5.228
[44] S.E. Totsuka Sutto, Y.I. Rodríguez Roldan, E.G. Cardona Muñoz, T.A. Garcia Cobian, S. Pascoe Gonzalez, A. Martinez Rizo, M. Mendez del Villar, L. Garcia Benavides, Efficacy and safety of the combination of isosorbide dinitrate spray and chitosan gel for the treatment of diabetic foot ulcers: A double-blind, randomized, clinical trial, Diab. Vasc. Dis. Res. 15 (2018) 348-351. https://doi.org/10.1177/1479164118769528
[45] M. Madrazo-Jiménez, Á. Rodríguez-Caballero, M.-Á. Serrera-Figallo, R. Garrido-Serrano, A. Gutiérrez-Corrales, J.-L. Gutiérrez-Pérez, D. Torres-Lagares, The effects of a topical gel containing chitosan, 0, 2% chlorhexidine, allantoin and despanthenol on the wound healing process subsequent to impacted lower third molar extraction, Med. Oral. Patol Oral Cir. Bucal. 21 (2016) e696. https://doi.org/10.4317/medoral.21281
[46] M. Piran, S. Vakilian, M. Piran, A. Mohammadi-Sangcheshmeh, S. Hosseinzadeh, A. Ardeshirylajimi, In vitro fibroblast migration by sustained release of PDGF-BB loaded in chitosan nanoparticles incorporated in electrospun nanofibers for wound dressing applications, Artif Cells Nanomed. Biotechnol. 46 (2018) 511-520. https://doi.org/10.1080/21691401.2018.1430698
[47] A.M. Cardoso, E.G. de Oliveira, K. Coradini, F.A. Bruinsmann, T. Aguirre, R. Lorenzoni, R.C.S. Barcelos, K. Roversi, D.R. Rossato, A.R. Pohlmann, Chitosan hydrogels containing nanoencapsulated phenytoin for cutaneous use: Skin permeation/penetration and efficacy in wound healing, Mater. Sci. Eng. C Mater Biol Appl. 96 (2019) 205-217. https://doi.org/10.1016/j.msec.2018.11.013
[48] A. Maged, A.A. Abdelkhalek, A.A. Mahmoud, S. Salah, M.M. Ammar, M.M. Ghorab, Mesenchymal stem cells associated with chitosan scaffolds loaded with rosuvastatin to improve wound healing, Eur. J. Pharm. Sci. 127 (2019) 185-198. https://doi.org/10.1016/j.ejps.2018.11.002
[49] P. Nordback, S. Miettinen, M. Kääriäinen, A. Haaparanta, M. Kellomäki, H. Kuokkanen, R. Seppänen, Chitosan membranes in a rat model of full-thickness cutaneous wounds: Healing and IL-4 levels, J. Wound Care. 24 (2015) 245-251. https://doi.org/10.12968/jowc.2015.24.6.245
[50] F.D. de Sousa, P.D. Vasconselos, A.F.B. da Silva, E.F. Mota, A. da Rocha Tomé, F.R. da Silva Mendes, A.M.M. Gomes, D.J. Abraham, X. Shiwen, J.S. Owen, Hydrogel and membrane scaffold formulations of Frutalin (breadfruit lectin) within a polysaccharide galactomannan matrix have potential for wound healing, Int. J. Biol. Macromol. 121 (2019) 429-442. https://doi.org/10.1016/j.ijbiomac.2018.10.050
[51] R. Ghosh Auddy, M.F. Abdullah, S. Das, P. Roy, S. Datta, A. Mukherjee, New guar biopolymer silver nanocomposites for wound healing applications, Biomed. Res. Int. 2013 (2013). https://doi.org/10.1155/2013/912458
[52] M. Goh, Y. Hwang, G. Tae, Epidermal growth factor loaded heparin-based hydrogel sheet for skin wound healing, Carbohydr. Polym. 147 (2016) 251-260. https://doi.org/10.1016/j.carbpol.2016.03.072
[53] Y. Liu, S. Cai, X.Z. Shu, J. Shelby, G.D. Prestwich, Release of basic fibroblast growth factor from a crosslinked glycosaminoglycan hydrogel promotes wound healing, Wound. Repair. Regen. 15 (2007) 245-251. https://doi.org/10.1111/j.1524-475X.2007.00211.x
[54] G. Eke, N. Mangir, N. Hasirci, S. MacNeil, V. Hasirci, Development of a UV crosslinked biodegradable hydrogel containing adipose derived stem cells to promote vascularization for skin wounds and tissue engineering, Biomaterials. 129 (2017) 188-198. https://doi.org/10.1016/j.biomaterials.2017.03.021
[55] G. Giusto, C. Vercelli, F. Comino, V. Caramello, M. Tursi, M. Gandini, A new, easy-to-make pectin-honey hydrogel enhances wound healing in rats, BMC Complement Altern. Med. 17 (2017) 266. https://doi.org/10.1186/s12906-017-1769-1
[56] M. Yang, Y. Wang, G. Tao, R. Cai, P. Wang, L. Liu, L. Ai, H. Zuo, P. Zhao, A. Umar, Fabrication of sericin/agrose gel loaded lysozyme and its potential in wound dressing application, Nanomaterials. 8 (2018) 235. https://doi.org/10.3390/nano8040235
[57] H.S. Koop, R.A. de Freitas, M.M. de Souza, R. Savi-Jr, J.L.M. Silveira, Topical curcumin-loaded hydrogels obtained using galactomannan from Schizolobium parahybae and xanthan, Carbohydr. Polym. 116 (2015) 229-236. https://doi.org/10.1016/j.carbpol.2014.07.043
[58] M.Z. Bellini, C. Caliari-Oliveira, A. Mizukami, K. Swiech, D.T. Covas, E.A. Donadi, P. Oliva-Neto, A.M. Moraes, Combining xanthan and chitosan membranes to multipotent mesenchymal stromal cells as bioactive dressings for dermo-epidermal wounds, J. Biomater. Appl. 29 (2015) 1155-1166. https://doi.org/10.1177/0885328214553959
[59] L. Upadhyaya, M. Semsarilar, D. Quémener, R. Fernández-Pacheco, G. Martinez, R. Mallada, I.M. Coelhoso, C.A. Portugal, J.G. Crespo, Block copolymer based novel magnetic mixed matrix membranes-magnetic modulation of water permeation by irreversible structural changes, J. Memb. Sci. 551 (2018) 273-282. https://doi.org/10.1016/j.memsci.2018.01.032
[60] D.R. Goudie, M. D’Alessandro, B. Merriman, H. Lee, I. Szeverényi, S. Avery, B. D O’Connor, S.F. Nelson, S.E. Coats, A. Stewart, Multiple self-healing squamous epithelioma is caused by a disease-specific spectrum of mutations in TGFBR1, Nat. Genet. 43 (2011) 365. https://doi.org/10.1038/ng.780
[61] X. Li, K. Nan, S. Shi, H. Chen, Preparation and characterization of nano-hydroxyapatite/chitosan cross-linking composite membrane intended for tissue engineering, Int. J. Biol. Macromol. 50 (2012) 43-49. https://doi.org/10.1016/j.ijbiomac.2011.09.021
[62] I. Garcia-Orue, J.L. Pedraz, R.M. Hernandez, M. Igartua, Nanotechnology-based delivery systems to release growth factors and other endogenous molecules for chronic wound healing, J. Drug Deliv Sci. Technol. 42 (2017) 2-17. https://doi.org/10.1016/j.jddst.2017.03.002
[63] S. Zahid, H. Khalid, F. Ikram, H. Iqbal, M. Samie, L. Shahzadi, A.T. Shah, M. Yar, A.A. Chaudhry, S.J. Awan, Bi-layered α-tocopherol acetate loaded membranes for potential wound healing and skin regeneration, Mater. Sci. Eng. C Mater. Biol. Appl. 101 (2019) 438-447. https://doi.org/10.1016/j.msec.2019.03.080
[64] X. Liu, L. You, S. Tarafder, L. Zou, Z. Fang, J. Chen, C.H. Lee, Q. Zhang, Curcumin-releasing chitosan/aloe membrane for skin regeneration, Chem. Eng. J. 359 (2019) 1111-1119. https://doi.org/10.1016/j.cej.2018.11.073
[65] T. Krupp, B.D. dos Santos, L.A. Gama, J.R. Silva, W.W. Arrais-Silva, N.C. de Souza, M.F. Américo, P.C. de Souza Souto, Natural rubber–propolis membranes improves wound healing in second-degree burning model, Int. J. Biol. Macromol. 131 (2019) 980-988. https://doi.org/10.1016/j.ijbiomac.2019.03.147
[66] A. Madni, R. Khan, M. Ikram, S.S. Naz, T. Khan, F. Wahid, Fabrication and characterization of chitosan–vitamin c–lactic acid composite membrane for potential skin tissue engineering, Int. J Polymer Sci. 2019 (2019). https://doi.org/10.1155/2019/4362395
[67] G. Ajmal, G.V. Bonde, S. Thokala, P. Mittal, G. Khan, J. Singh, V.K. Pandey, B. Mishra, Ciprofloxacin HCl and quercetin functionalized electrospun nanofiber membrane: fabrication and its evaluation in full thickness wound healing, Artif Cells Nanomed Biotechnol. 47 (2019) 228-240. https://doi.org/10.1080/21691401.2018.1548475
[68] R.S. Sequeira, S.P. Miguel, C.S.D. Cabral, A.F. Moreira, P. Ferreira, I.J. Correia, Development of a poly(vinyl alcohol)/lysine electrospun membrane-based drug delivery system for improved skin regeneration, Int. J. Pharm. 570 (2019) 118640. https://doi.org/10.1016/j.ijpharm.2019.118640
[69] B.C. Garms, F.A. Borges, N.R. de Barros, M.Y. Marcelino, M.N. Leite, M.C. Del Arco, S.L. de Souza Salvador, G.S. Pegorin, K.S.M. Oliveira, M.A.C. Frade, R.D. Herculano, Novel polymeric dressing to the treatment of infected chronic wound, Appl. Microbiol Biotechnol. 103 (2019) 4767-4778. https://doi.org/10.1007/s00253-019-09699-x
[70] X. Li, Z. Cai, D.U. Ahn, X. Huang, Development of an antibacterial nanobiomaterial for wound-care based on the absorption of AgNPs on the eggshell membrane, Colloids Surf. B Biointerfaces. 183 (2019) 110449. https://doi.org/10.1016/j.colsurfb.2019.110449
[71] J. Shao, B. Wang, J. Li, J.A. Jansen, X.F. Walboomers, F. Yang, Antibacterial effect and wound healing ability of silver nanoparticles incorporation into chitosan-based nanofibrous membranes, Mater. Sci. Eng C Mater Biol App. l98 (2019) 1053-1063. https://doi.org/10.1016/j.msec.2019.01.073
[72] S. Pal, R. Nisi, M. Stoppa, A. Licciulli, Silver-Functionalized Bacterial Cellulose as Antibacterial Membrane for Wound-Healing Applications, ACS omega. 2 (2017) 3632-3639. https://doi.org/10.1021/acsomega.7b00442
[73] L. Tarusha, S. Paoletti, A. Travan, E. Marsich, Alginate membranes loaded with hyaluronic acid and silver nanoparticles to foster tissue healing and to control bacterial contamination of non-healing wounds, J. Mater. Sci. Mater Med. 29 (2018) 22. https://doi.org/10.1007/s10856-018-6027-7
[74] S.S.D. Kumar, N.K. Rajendran, N.N. Houreld, H. Abrahamse, Recent advances on silver nanoparticle and biopolymer-based biomaterials for wound healing applications, Int. J Biol. Macromol. 115 (2018) 165-175. https://doi.org/10.1016/j.ijbiomac.2018.04.003
[75] M. Naseri-Nosar, Z.M. Ziora, Wound dressings from naturally-occurring polymers: A review on homopolysaccharide-based composites, Carbohydr. Polym. 189 (2018) 379-398. https://doi.org/10.1016/j.carbpol.2018.02.003
[76] T. Krupp, B.D. dos Santos, L.A. Gama, J.R. Silva, W.W. Arrais-Silva, N.C. de Souza, M.F. Américo, P.C.J.I.de Souza Souto, Natural rubber-propolis membrane improves wound healing in second-degree burning model, Int. J. Biol. Macromol. 131 (2019) 980-988. https://doi.org/10.1016/j.ijbiomac.2019.03.147